Blog Posts:
**The posts are in chronological order so the beginning is at the very bottom and the most recent is at the very top. You can navigate the posts by using the arrow at the bottom to see older posts.**
Click here to be brought to the beginning story.
Content Warning: Blog posts cover weight, eating habits, and medical experiences which may be triggering for some readers.
*All medical teams and hospital names have been excluded from all stories for privacy reasons. *
~ Scroll to the bottom to see the ‘Older Posts’ arrow to navigate past postings. ~
Small Sips Still Equals Big Flares
So, my spring break had just begun, and my GI doctor wanted me to trial the enteral feeding formula soon to know if they could transition me to enteral feeding in the summer.
I still had some of my enteral feeding formula drinks from over the summer when I had tried them prior to being admitted. They still weren’t expired yet, but the date was coming up, so I felt it was necessary to try them soon and if anything happened, I wouldn’t be missing school at least.
At 11:30am on March 6th, I took 1 sip of the enteral feeding formula and immediately went into a dry heaving fit afterwards.
I did manage to swallow it down and it did stay down even among the dry heaving fits.
2o minutes later my nausea still was increasing but I tried to ignore it and rested in bed watching Netflix.
At 12:40pm my pain had escalated so high that I needed to take my oxycodone.
At 12:45pm I took my nausea medication and talked on the phone with my dad.
I spoke with my dad about feeling frustrated with myself for trying the enteral feeding when we all knew it was going to make me flare.
I felt frustrated that I kept naively trying foods/drinks while my doctors were just there to recommend me to try something else while I was left to suffer the consequences of it for such long periods of time.
I had more dry heaving fits into the evening and took more nausea medication at midnight.
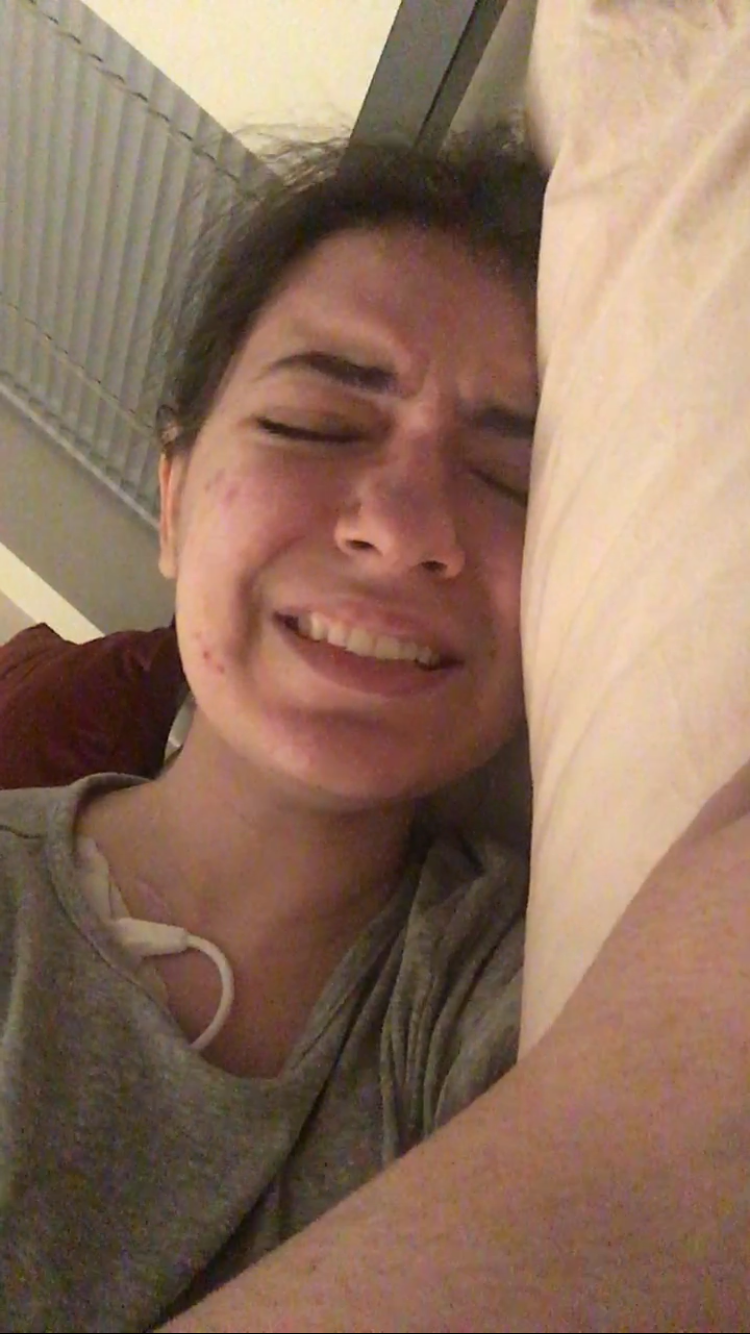
I had gotten up to be in the night and was crying from how bad the pain had gotten.
I couldn’t even roll over in bed without crying- interesting reminder from the past, when this exact scenario happened in Texas (As mentioned in “The Hell Weeks”).
I sent off an email to my medical team that evening regarding my thoughts on these “food trials”. I have an image of the email below with names redacted for privacy.
I was up all night with the flare and got a few hours of sleep finally at 7 am the next day.
I wasn’t as hunched over the following day, but my nausea was still so incredibly high.
I continued taking my nausea medications and had to take another oxycodone for the spikes in pain that began midday.
My nurse had also happened to come that day to change my dressing and I once again unlocked the door from my phone in my bed.
As the evening came, my flare escalated, and I had to take another oxycodone.
This was the most I had taken oxycodone in sequence to each other. Normally I’d just have 1 at the height of the flare but this flare just wasn’t giving up.
I was up all night once again for the second night in a row- really not loving that.
Spent all day of March 8th in bed but luckily didn’t need to take any oxycodone.
March 9th I was able to shower but had a dry heaving fit afterwards from doing so.
This day my stool also became very irregular.
I also had gotten in the mail a rug that I had ordered for my new apartment which I was excited about being able to have a space to design soon.
March 10th, I spent all day in bed and my flare was de-escalating, just really slowly.
March 11th I was awake most of the night with diarrhea. I had an appointment with hematology in the morning and for some reason my fatigue and sugars were really awful. I almost passed out multiple times on the journey there and my whole body was shaking.
My period began midday which was making my blood sugars fluxuate even more than usual.
I had gotten more labs done during my appointment and kept arguing with the nurse practitioner to explain that my liver issues were because of my TPN, and my anemia was because of eating iron.
They still didn’t believe me for either, but I had told them that when they saw the results of my liver enzymes, they’d be lower because we adjusted my TPN (proving that the liver issues are connected to my TPN).
I received a call late in the afternoon with the nurse practitioner explaining to me that I likely didn’t have porphyria and didn’t need to continue with genetic testing because my liver issues were because of my TPN. – Wow, took the words right out of my mouth.
Got one point across but I still have to work on the anemia explanation though-we’re getting there…
The following day I was finally feeling back to normal and was able to work on some schoolwork and rest unfortunately just as spring break was ending.
The flare from the enteral feeding formula lasted a total of 6 days.
Read what happens next in, “Back in the Norm and Prepping to Move!”
Shows, Blood Labs, What Else Is New?
After my egg flare had ended, things seemed to be going back to normal mostly aside from just having more tremor issues.
My hands would shake so much in the evenings, so I learned to never do classwork then because my hands were too difficult to function with.
I went back to rehearsals on February 22nd, and it was so nice to be back there with everyone.
I had also noticed that every time I returned home from rehearsals, my blood sugar would drop significantly from all the energy it took while I was there to “appear okay”.
To combat this, I just started taking my glucose tablets more frequently at rehearsals.
I was a bit bummed about the theatre rehearsals because I had wished that I was able to do more and help out more, but I just wasn’t at the place physically to be able to.
It took some time to cope with and was one of the hardest parts of returning to the theatre.
A couple of the rehearsals I had the most embarrassing thing happen- my pump alarmed. *Insert disappointed face here*
It was SO NOTICABLE and one of the times it happened to be in a tech rehearsal which felt so disruptive.
Both times it was because of “sticky keys”. -This, this right here is why I miss my other pump.
Gertrude has a vengeance for me I swear, and she loves to be noisy when I least expect it.
One of the rehearsals I got to run a production meeting which was such a wonderful semblance of how things used to be. I felt helpful and it reminded me of who I was as a stage manager which I hadn’t felt in so long.
The show ended up looking really cool and I was so glad to have been a part of it (even if I was out sick for a lot of my job).
On March 1st it was midterms for my first 2 classes, and I was so proud of myself for making it so far into the semester.
I also had a GI appointment that morning (the first one since my dad left) and it was meh. The good news was that my liver enzymes were going down since alternating between the non-lipid and lipid TPN bags.
The doctor said I didn’t need to do the liver biopsy and that I didn’t need to get enteral feeding in April.
Whew!
They did however mention that they wanted me to trial the enteral feeding formula (the drink) and specifically mentioned for me to have, “ONE sip”. The doctor said they figured it would likely cause a flare because the enteral feeding formulas have a lot of components and nutrients in them.
Great-looking forward to it.
They had also mentioned that they wanted to schedule an endoscopy and colonoscopy to be done in April (which I was going to move to the summer). I asked why they wanted to do a 3rd endoscopy and they said that they hadn’t seen it for themselves and wanted to do the procedure themselves.
On March 2nd I began reintroducing food back into my diet since I figured the egg flare was far enough away that I felt comfortable retrying some of my other “safe” foods.
I had gone to the pharmacy and picked up some Sweet Tarts on my search for Smarties (still not sold anywhere…). They went okay-similarly to the Nerds, but I ate less of the Sweet Tarts because my stomach would hurt sooner so I’d snack on a few throughout the day and let them melt on my tongue.
I worked on my final 3D model for my scenic class as I entered into spring break!!
On March 4th I wrote out a seven paged letter that I read to my family and worked on editing to send to my medical team regarding my medical care moving forward and where I wanted to go from there.
It was an emotional day but a very important one because I made a lot of steps in understanding where to go next with advocating for myself.
Read what happens next as Emma trials the enteral feeding formula in, “Small Sips Still Equals Big Flares”.
Egg the Size of A Cheerio…
February 13th, I began my day by eating some Nerds which had been going pretty okay. For me, any food I ate would cause pain and me to regret it later, but it generally didn’t cause a flare (defined by me as immobilized in bed for a minimum of a week) so my brain took that as it was still “fine” to eat.
I was just going about my day doing some cleaning around the house and had a pretty normal morning. I did have a random vertigo attack as I was cleaning so I just figured the air pressure must’ve been changing outside.
I showered and then rested on my couch watching that Netflix show I had gotten hooked on.
As I was watching TV, my hunger craving started appearing.
I want to define here that my hunger cravings are simply psychological cravings for the pleasure of eating and not for the nutritional or literal need of eating. My TPN fully nourishes me so anything I get in is considered a “bonus”.
I had wanted something more, something “heftier” to eat that was more than the peanut butter.
I then thought back to my time in the hospital when I had eaten blended up versions of food.
Aha! I’ll try blended up scrambled eggs!
I really wanted eggs and I knew how to make it super plain.
I was so excited because after I got the eggs into my mind, I could already practically taste it and it was just what my mind wanted to eat.
I cracked 1 egg into a bowl, scrambled it with a fork, and stuck it in the microwave to cook it (I used to do this every day for breakfast during my whole freshman year of college in my dorm).
After making sure it was fully cooked (it was pretty dry) I then grabbed a blender and blended it down until the egg was in super tiny pieces.
I added a little bit of salt and put some into a bowl (I overserved myself because I forgot that I couldn’t eat regular meals).
At 2:45pm I began eating 2 bites of the egg that were so small I could dissolve the pieces with my tongue. The pieces together would’ve been about the size of a cheerio.
I waited after those 2 bites (very challenging to restrain) to see if my body had any reactions before I kept eating.
I was distracted and watching my Netflix show the whole time (in the background) that I was very hooked on.
A minute later (2:46pm) I began getting sharp epigastric pain which prompted me to put the bowl of egg away so I didn’t eat more since I wasn’t sure if the pain was going to escalate (and I knew eating more would make it escalate).
After throwing the bowl of egg away, I sat back on the couch to watch my show.
At 3:11pm, I began feeling much more noticeable abdominal pain which made it hard to focus on my show. However, I was stubborn and wanted to keep watching so I managed to keep switching my focus back to the TV.
At 3:20pm I had to sprint to the bathroom to have diarrhea (likely from earlier or yesterday’s food and not from the egg; the egg moving through my system likely prompted a bowel movement).
At 3:30pm I had to shut the show off to take an oxycodone because I could no longer watch TV due to the intensity of the abdominal pain.
After taking the oxycodone, my pain dropped to its usual levels (a 7) and I wrote an essay on my couch that I needed to work on for class.
I got up off the couch at 5:40pm when my alarm went off to change my TPN.
I washed my hands, got my supplies out and prepped my vitamins.
After injecting the vitamins into the TPN bag, I was suddenly hit with vasovagal syncope-like reaction.
My eyes got really watery, and my face went pale. I immediately grabbed my phone (which is why my phone is ALWAYS on me- for medical emergencies like this because they always come out of nowhere) and dialed my dad.
In the process of dialing the phone I immediately dropped to the floor as I was hit with the most massive wave of nausea. My vertigo was also acting up alongside everything else which prompted me to keep my eyes closed. My stomach began hurting REAL bad and was swelling up like a balloon. I took my nausea medication at 5:55pm to no avail because I began vomiting shortly after.
I couldn’t really move, and my dad was on the phone trying to keep me calm and make sure that if I needed help and couldn’t dial 911, he would.
I kept vomiting over and over and the first round of vomit was- you guessed it, my 2 pieces of egg from 2:40pm earlier that day. Wild right?
That’s gastroparesis for you!
Since I still hadn’t really been able to open my eyes and DEFINITELY could not stand up- I had reached for a cardboard box by the trash to vomit in.
The remainder of the vomiting cycles were mostly clear so that was good.
After the vomiting I remained curled up laying on the floor with the vomit box next to me and my phone by my head with my dad on the other end with my eyes still closed.
As I was trying to keep myself calm, I talked to my dad about the characters from the Netflix show I had been watching. It helped in between the vomiting cycles.
At 7:10pm (AN HOUR LATER), I was able to move my TPN stuff to the floor to finish changing my TPN.
I had opened my eyes and realized my vomit box was leaking on the kitchen floor-great.
I somehow managed to get up (hunched over) and clean up the vomit and throw it out in the trash chute (because I had been in my apartment before with vomit in the trash and it can really stink up the place).
I hung up the phone with my dad and crawled into bed. I put on Netflix on my laptop and tried to determine whether I felt up to going to school the next day.
At 10pm that evening I took my pills without my muscle relaxer (just dealt with the esophagus pain) because I didn’t want the muscle relaxer to inhibit my vomiting if my body needed to vomit again.
February 14th, the next day.
My body really wanted to remind me that it’s in charge and that I should not be eating.
I woke up at 8:30am from my alarm and was in SO much pain. I had gotten out of bed to use the bathroom and the act of standing up made things immensely worse.
I emailed my professors that I wouldn’t come into class, but I’d attend virtually.
As I tried to change out of my pajamas, I began a dry heaving fit.
I took another oxycodone at 9:17a.m.
Pain however, kept escalating.
I tried my best to do my schoolwork, but my body just was not having it and strongly disliked that I was disobeying it.
I began vomiting again from doing too much classwork.
I took nausea medication, but the vomiting continued.
I quickly raced to my apartments front door carrying a trash bag-still vomiting from all the movement- to unlock the door so if I needed to call 911, they could get in by me unlocking the door with my phone.
I made it back to my bed and kept vomiting because again, movement is my worst enemy in these flares.
All of my symptoms flared up from this; I had so much acid reflux, my fatigue was awful, I began getting migraines, and my esophagus spasms were heightened.
My nurse came to visit me late in the afternoon to change my dressing and I unlocked the door from my phone since I couldn’t get up.
That evening I stopped vomiting but still had dry heaving fits with movement.
I had to email my school because the theatre show I was assigned to had me specifically working that week. Since I couldn’t move, I couldn’t go to classes or rehearsals.
It was very frustrating.
The flare from the eggs lasted 8 days long.
There’s too much that occurred every day to be able to write it all in this article but just know the days were spent how they were in the summer. The only difference is it was shorter because I didn’t continue eating whereas in the summer, I did because I didn’t know that food was making it worse.
Towards the end of the flare, I did catch up on schoolwork (I didn’t have much because I work ahead naturally so that ended up aiding me) but had a lot of fatigue troubles and tremor issues (which was hard because I was making a 3D model and my hands kept shaking).
Read how Emma recovers after her egg flare in, “Shows, Blood Labs, What Else Is New?”
Hunger Cravings
In this story I begin the use of the acronym, “G.T.A.F.” which stands for “got tricked, ate food”.
I actually first heard this term used by someone on their blog when I first was having issues with coping with the fact of not eating. I’ll link the blog post I found it from here: https://findingmymiracle.com/2016/02/09/when-you-cant-eat-part-one-the-facts/ ).
I began having my stomach grumble during classes and it especially occurred in the evening.
It began once I started changing to my non-lipid bags because those bags didn’t contain fats.
Since then, my stomach still grumbles even today (just less).
Anyways, back to the story,
On February 6th, I had a moment where I suddenly had a hunger craving which meant my brain was suddenly wanting food urgently and I then started having my stomach grumble. My sense of smell had been SUPER heightened since stopping eating back in August, but it was practically smelling everything in my kitchen from my bedroom.
I was trying to continue doing my homework, but the craving was so strong that I couldn’t hold back, so, I went into my kitchen and started looking.
I kept grabbing things and smelling them, which was pretty weird but luckily my roommate wasn’t home from work yet-lol.
I grabbed some baby food that I had in my pantry from months ago (when I was able to eat) and tried some of the non-expired ones.
I was bummed that all of them were so “sweet-tasting”. I really wanted a vegetable flavored one.
I first tried a lick of the apple and carrot, then a lick of vegetables and pear, and then 2 licks of apple and broccoli because that one tasted and smelled the best.
Since I was still wanting savory, I grabbed some table salt and poured it on my finger and licked it- better.
My body was craving more food and began shaking just from the psychological reaction of having some of it. The shaking was the kind of shaking that happens when you’re really starving and need food. It was pretty uncomfortable because I just wanted to open the fridge and eat a hamburger, or a steak, ooh or a sandwich with turkey and a side of pickles….
AHH,
I’m getting distracted…. Where was I…
Ah yes, the hunger cravings.
I luckily remained fairly unscathed and had a minor flare later in the evening which then coined me using the term G.T.A.F.
I did in fact have to let my roommate know when they got home, that I did in fact, “get tricked, [and] ate food”.
February 7th, I arrived home from my classes and once again had that hunger craving for something “heavier” that would satisfy my craving. So, I thought of peanut butter.
My previous roommate had a squeezable version of peanut butter which I figured would be better to use since I could control more of the amount I was taking in (because we all know I would’ve taken spoonsful of peanut butter out of the jar otherwise).
I once again G.T.A.F., and took my time eating 2 little dollops/sections of peanut butter on a spoon.
The taste was impeccable- given, I hadn’t eaten anything in so long that rice would’ve been impeccable.
It unfortunately did cause more digestive issues because there was a bit more to peanut butter as compared to candy, but the taste was making it difficult for me to give it up just yet.
My fatigue continued to worsen into the next day with me having to hold onto the railings in the hallway of the hospital as I took standing breaks.
I had another spoon with some peanut butter on it for the day which was the time I was always most excited for.
At 11:21p.m. that evening my stomach was grumbling because it knew that peanut butter was sitting in the pantry in the next room…
I got a call the following day from hematology saying I did not have the acute intermittent porphyria gene, but they wanted to run a panel for all of the other porphyria genes. -I told them I’d talk to them about it at another time.
February 9th, I began upping my peanut butter spoon intake because once again the flavor is just too tough to beat, and I yearned for something savory.
I began having 4 peanut butter spoons (a line of peanut butter on a spoon) and would take about 10-20 minutes to eat each one to savor the flavor.
On February 10th and 11th I went back down to 2 spoons of peanut butter because I was busier during the day but I lived the consequences for reintroducing food into my diet because in the evenings I had to sleep upright again with the heavy levels of acid reflux I was getting (even on all of my acid reducers!!). So much acid up into my nose :-( .
February 12th, I started watching a new series on Netflix which was pretty good, but my peanut butter companion was no longer satisfying my hunger craving.
My body wanted more… much more…
Read what happens next in, “Egg the Size of A Cheerio…”
*I also have an article in Advice & Thoughts which goes into more of the psychology behind hunger while being fully nourished. It’s titled “My Thoughts On the Psychology of Long Term Hunger Cravings”.
Shower Shakes & Fatigue
On January 27th, I had to head to the hospital to get my abdominal ultrasound done to check on how my liver and gallbladder was doing since my liver enzymes were continually elevated.
I had some trouble finding where I needed to go in the hospital and people weren’t super helpful in helping me find my way there. :-/
My appointment was at 7:30 in the morning and I had class later in the day which I was already feeling really exhausted for.
The ultrasound was fairly short, but it gave me quite a lot of abdominal pain and nausea since they have to press the wand into your abdomen to get a good reading. I went home with my pain spiking knowing my entrapped nerves were likely also triggered.
I got home at around 8a.m. and received an email that my class had been canceled!!
At around 10a.m. I went to a different hospital to go get my labs done for my autonomic neurologist. The blood lab office was so packed with people, and it took an hour and a half in the waiting room!
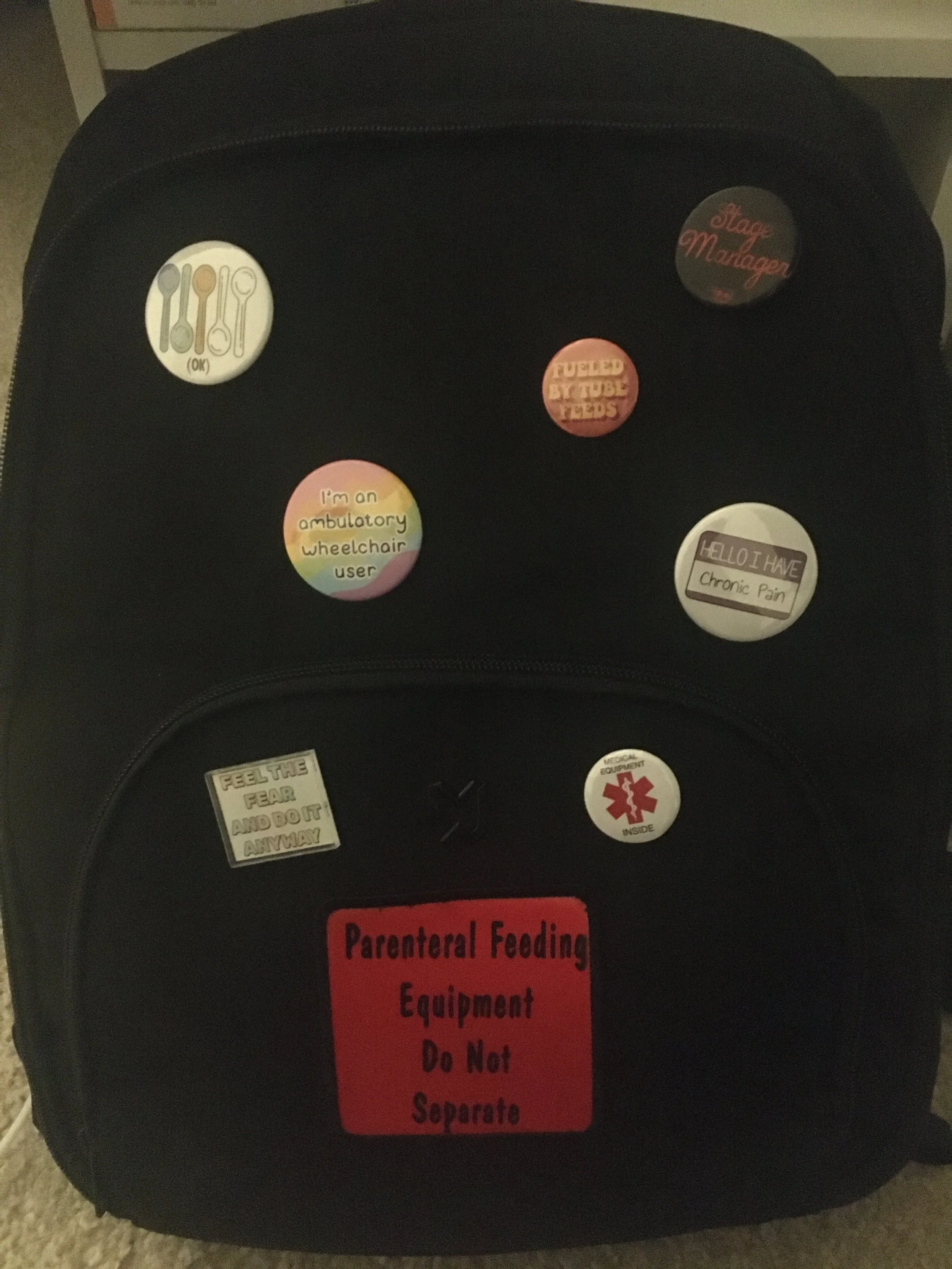
Luckily, I didn’t have anything else on my agenda, so I didn’t mind the wait. It was a bit awkward though because most of the patients in the room were much older than I was, but they were all staring at me and the backpack. Definitely a scenario where I practiced not being bothered by the stares!
At 5:40p.m. while I was in the middle of disconnecting my TPN, I suddenly had a super sharp abdominal pain deep at the bottom center of my rib cage (around where my hiatal hernia is) and had to sit down on the floor from the pain/nausea.
I laid down on the kitchen floor since the pain kept escalating and took a Zofran for my nausea. I had to remain on the floor for 40 minutes until I could sit up again. I had called my dad on the phone and pulled my TPN bag to the floor so I could change it there.
I quickly reconnected at 6p.m. and continued remaining on the floor.
My abdomen began swelling at about 6:50p.m. so I removed my tank top since it was becoming too tight and leaving a mark around my epigastric region.
At 7 p.m. I had enough and knew I was either taking ½ an oxycodone or going to the ER. I knew I’d be turned away at the ER, so I took ½ of my oxycodone pill. Luckily, after 10 minutes I was now able to stand up from the kitchen floor and make it to my bed.
I didn’t take my nightly pills that evening because I usually have to take my muscle relaxers to be able to swallow the others. I have an app that measures pill interactions (so I know what things might interact with each other) and it said my oxycodone was not safe to take with the muscle relaxer. Therefore, no pills that night.
I spent most of the day in bed the following 2 days.
On January 30th I had taken a shower but accidentally spent too much time inside (about 15min). I could tell because mid-shower my hands started shaking.
I got out of the shower and took my glucose level and it had dropped to 89 (it was usually in the 100s while connected to TPN). I had to take my glucose tablets and sit and wait until my body stopped shaking.
From this point on I knew I needed to be more careful and try to shorten the time I was in the shower as much as possible.
On January 31st I had received a call from my GI doctor who went over the results of the liver ultrasound with me. They let me know that I had stage 1/mild steatosis (fatty liver disease) and biliary sludge. They said they spoke to a hepatologist (liver specialist) and said that my gallbladder didn’t seem inflamed so at the moment I don’t need surgery to remove it.
They just wanted me to continue trialing the non-lipid TPN bags and we’d see how my liver would respond.
Later that day I had spoken with my parents, and we discussed the whole moving apartments situation. We figured that since 1-bedroom places in the area were all generally the same price as the one bedrooms in the building I was already living in, we’d keep me in the same building since it’d be easier for me to move a few floors rather than a whole new building (having to hire movers, etc.).
We had found some 1-bedroom floor plans in my building, so I spent my free time over the coming months, drawing up floor plans and designing the space on paper.
On February 1st I was still having a lot of issues with fatigue and blood pressure being low. One of my blood pressure readings from that day after arriving home from walking back from class was 94/52 which was quite low for me especially after physical activity.
I had also noticed over the coming days that since changing to lipid and non-lipid bags I was having more issues with constipation which was another unfortunate side effect.
On February 4th I had my next appointment with my primary care physician however, my building shut down all their elevators without telling anyone.
I had to call the building, the manager etc. to get help getting downstairs since I still couldn’t walk downstairs. It was a bit annoying that the building hadn’t thought of that, and I had went ahead and called the doctor’s office to let them know I’d likely be late- since me calling the building had already taken 20 minutes!!
The office receptionist said I had to arrive within 10 minutes of my appointment or else it would be cancelled!
Oh boy- a challenge.
I FINALLY got downstairs after the building manager met me on my floor with the freight elevator. I raced all the way to the hospital with my feet killing me and my heart rate beating through the wall. BUT, I did in fact MAKE IT.
I spent my time in the waiting room trying to catch my breath.
It was a fine appointment and was mostly a check-in.
They told me that with elevated liver enzymes, Porphyria labs can look falsely elevated- which you know I made sure to remember for the next time I saw hematology.
After the appointment I spent the rest of the evening at home resting in bed and worked on inspiration and designs for the future apartment.
Read about Emma’s new hunger issue in, “Hunger Cravings”.
Finding the Limits
Feeling frustrated about that cliffhanger huh?
I added that in there to have you as the reader feel some of the craziness I felt in that appointment!
My dad and I were obviously very opposed to enteral feeding since we figured having things run through my digestive system (the thing that put me on a central line in the first place) would be a bad idea.
They said the only other option would be a trial of me not being on TPN for a week, but it would be very rough since I wouldn’t have nutrition.
In all honesty, I was much more willing to do the “not on TPN for a week” than enteral feeding. I just kept a mental note that I’d likely need to be admitted since it’d be pretty dangerous to monitor on my own.
After they gave me that information in the appointment, they also said we were going to do an esophageal manometry and that it’d be very uncomfortable, and I’d have to be awake. They said that this either finds that my swallowing issues are fine, or they find that they’re nerve related in which case, they can’t do anything to fix it (which made me consider for later if I even wanted to do this).
They did a repeat of labs to check my liver enzymes which unfortunately all grew higher in number. This also resulted in hematology being very confused as to why I also had my anemia. This began the endless explanation of me trying to explain that not eating anything with iron for 6 months will result in not having iron equaling anemia.
I left and would see GI again in March to “enact” one of these plans… great…
Off to class!!- First in person class too!! It went really well but I had trouble figuring out how to place my backpack in a spot where people wouldn’t trip over my line. Made me pretty nervous anytime anyone stood up to walk around the aisles.
Also, for this first day of in person classes I did use my old CADD Solis tubing which was very helpful.
I got home and saw that my dad and roommate had a little surprise for me from doing my first in person class.
I had still also been going to physical therapy at this time (once a week) and my visiting nurse still came to my house every week.
My second day of in person classes was with my other classes I hadn’t seen yet. It was a bit more challenging because, I didn’t have as many places I could set my backpack and the pump was also audible which made me so embarrassed too.
It was a bit weirder in person interacting with peers since it was so evident that things had changed. This was one of the largest challenges with coming back to school.
It definitely felt like I had lost time or that I was “behind”.
I had a hematology appointment after class and once again tried to explain to them how anemia happens, but it wasn’t working. I also was told that the hematology team thought I had some form of Porphyria (a rare blood disease). They thought I specifically had acute intermittent porphyria and had my labs sent off to Mayo clinic to be gene tested.
I had been tested for porphyria 3 times before and did not have it, so I wasn’t sure why they were so adamant on it. They said my most recent urine sample showed some markers for one of their porphyria tests (but my past urine tests during my flares hadn’t).
Later that day I had also gotten a call from my nutritionist detailing out a new TPN plan that I wish I had been informed of before all of the giant leaps during my past appointment. They said I would be getting new “non-lipid” TPN bags for 3 days out of the week. Therefore, I’d be alternating from lipid to non-lipid bags throughout the week which would hopefully give my liver more of a break.
January 21st, I had gotten my second iron infusion, but I was still so fatigued and wasn’t feeling any better. The doctor’s mentioned that since my red blood cell count was so low, it’d likely take months to get it back to where it used to be to feel normal again.
It was also a really significant day on January 21st because that evening my dad left back to Texas. My dad had been living with me at this point for 6 months and had also become great friends with my roommates (which at this point only one remained still at the apartment since the other moved). It was a sad goodbye for everyone, but it was a good sign that things were moving in the right direction.
January 22nd, I began on my new “non-lipid” TPN bags which looked like yellow Gatorade. It was really hard to prime the tubing because the liquid when it isn’t all together appears clear.
Classes were going good and it was nice to have some time in my day to escape and feel like I wasn’t sick. Often times class would make me forget about it and it was nice at that time.
On January 24th I headed to my first rehearsal since getting sick which I was really worried about being able to handle. I had to go to rehearsal after my TPN change time, so my backpack was FIFTEEN POUNDS. Oh boy it was a noticeable weight.
My shoulders were always bothering me when I had rehearsals because of how heavy the bag was. It definitely took time to get used to.
It was a great time being back at rehearsals, but it made me realize very blatantly how much I missed theatre and how much I couldn’t do the things I used to do.
During this time at school, I was having to be much more cautious with my glucose because my sugars where always dropping with certain activities.
I went to the store to try and find some smarties to get to help with the sugar levels because I didn’t want to be having glucose tablets too often.
Unfortunately, none of my local stores sold smarties so I got the next best thing- Nerds?
I got pain after eating a few of them but it wasn’t a flare, so I considered eating them again the following day (as needed for low sugars).
On January 26th I had a virtual appointment with my autonomic neurologist which was perfect because I had also been having circulation issues for a couple months leading up to the appointment.
They went over the cervical spine MRI with me and said they didn’t think it had anything to do with my tremors but that it could be a rheumatology related issue, so they sent a referral for me to see one (I hadn’t seen one yet).
They also ordered more lab work for me to stop by the hospital some time to get it done.
After my appointment I had decided not to go to my next class because I had a huge fatigue wave hit and I couldn’t move much and was out of breath. I was glad that for the first time, I put myself first.
Later that day I also had used up my last CADD Solis tubing and had to ship back the pump to my supply company- Bye Steve, you will be missed.
The next day was set as a doctor filled day since I had to go to 2 different hospitals!
Read how those visits go in the story, “Shower Shakes & Fatigue”.
Liver Disease, Anemia, and Ready for School!
January 10th was a huge day, a day I had been aiming to make it to through my whole line of treatment.
The first day back at school.
I had gone through so many doctor’s saying I’d never be able to do it and that it wasn’t safe, etc., and here I was, following my own goals and going back to school.
It was the start of my sophomore spring semester at college, and I had virtual classes for the first 2 weeks.
I was happier about this than the usual population because it gave me an opportunity to gauge how much energy it would take to do class and how my physical pain would respond and react while trying to “look and act normal” in class.
The first virtual class went great, and it was the first time I was seeing my old peers on the camera. I was so nervous but also so excited to see them.
During my second class, I started having sharp abdominal pain midway through the class and it lasted for the rest of the time. I made it through trying my best to not show it but after the class ended, I sprinted to the bathroom and had a dry heaving spell.
I did my homework lying down in bed since I can’t sit up at a desk for very long.
I got really fatigued in the evening because I did too much work.
I ignored my fatigue (bad idea) and showered later that evening. I also accidentally cut my ankle a small bit when I was shaving, and I completely forgot that I was on blood thinners so this cut WOULD NOT STOP bleeding even after band aids and pressure (it did stop bleeding after the 2nd day, but it was a small cut, so it was more of an annoyance than concern).
The following day I had my next class which I was super excited about. It was an Ethics of Eating course which I took completely for the irony (also because I was curious about the psychology behind eating).
I woke up to be nauseous since I had tried to make my bed that morning. I also had a lot to do in the day like go to the pharmacy so I took a Lyft since I still couldn’t walk far. From doing too much yesterday and today I had a nausea and tremor attack midday as a consequence of overusing my energy.
It was still and IS still a very difficult thing for me to grasp that my body does not have ANY energy reserves. Even not doing a physical action but a mental one (such as reading) would result in just as much fatigue as walking would. -Still very hard for me to wrap my head around.
I had a meeting later that day with my school’s disability and accommodation center to get academic accommodations for my illness (since my flares were unpredictable).
*if you’re interested on more about how to go to school with TPN, read my Advice & Thoughts article titled, “Going to School with TPN”.
On January 12th I had to wear a sweater with my lumens on the outside of it because I had an infusion later in the day and it was winter, and I didn’t feel like undressing for the infusion for them to be able to get to my central line. I was super nervous with my outfit because it was the first time I was wearing visible lumens to my zoom classes, and I was so self-conscious about it.
I made it through class and was excited to FINALLY GET MY IRON INFUSION (had been waiting since AUGUST).
My dad and I went over to the infusion center, and they turned us away saying we had an “appointment” and not an infusion.
WHAT?!
We went to the other office, and it was in fact AN APPOINTMENT. They scheduled me for AN APPOINTMENT and not an infusion?!!
AGHHHH.
Anyways,
We met the nurse and doctor, and it was a really confusing time because I wasn’t prepared for the appointment because I thought it was an infusion (because I was told it was an infusion-go figure). They were asking me medical history etc. and I kept saying wrong things because I was in the complete wrong mindset and was not properly ready to explain 2 years of history.
Unfortunately, this did affect things.
They took labs, urine samples, blood pressures, orthostatics, etc. and I was given yet again another stool sample kit to take home to bring back.
Their team seemed really enthusiastic about figuring out what the illness was, but I thought to myself, “that’s cute, thank you but good luck”.
That evening I fell asleep at 6:10p.m. from all the fatigue from the day.
The next day I received multiple phone calls during class from the hospital. I turned my camera off on my virtual class and picked up the phone.
It was the hematologists and they said, “you are severely anemic, and we need you in the hospital to do an infusion like, now, so how soon can you get over here?”
OHHHHHH HO HO!!!!!!!!!!
YOU MEAN I’VE BEEN SEVERELY ANEMIC FOR MONTHS? And when my dad and I said this over, and over, and over again to get an infusion….we were correct all along?
Ah yes- the modern-day medical system.
So immediately after my class I headed to the hospital dropped off my stool sample and read through my lab reports in the infusion waiting room. Uh-oh, a lot of these labs were coming back not looking very good-and not just the anemia ones…
I had my infusion which went fine and then the hematology nurse practitioner came in to talk to me about my lab results. They said that ferritin levels for the average female my age was 30 and mine was 6.
Because it was so severely low, they said they gave me double the iron for my infusion and I’d have to come back next week to get another infusion.
It was also then that they informed me that my liver was not looking so good. My liver enzymes were INSANELY high and higher than normal for people on TPN (since it is usually expected to be elevated with those on TPN).
They didn’t say much else, but I went home feeling so exhausted.
I had gotten 4 hospital phone calls within 2 hours and had to re-sign my lease with my new roommate since the old one had left plus, I also had classwork from school.
Ah, the new balance of things.
On January 14th I received news from my GI team (because of the hematologists reaching out to them) that my LFTs (liver enzymes) had been steadily rising for months and they had been adjusting my lipids to try and stop them from continuing up. (-wow thanks for that heads up)
They said they wanted to talk more about it with me when I saw them on the 18th and wanted to do an ultrasound and potential liver biopsy.
I had also weaned off of Tylenol just to not make liver issues worse. The 14th was my first day entirely off pain medication and it was absolutely miserable. I was in bed unable to move and had so much nausea. I also had so much swelling and inflammation of my epigastric region and just tried to sleep.
The 14th-17th I was in such severe pain and symptoms were flaring so much that I just spent the day in bed trying to take it as best as I could. In my journals (which I use to write these) there’s such extensive notes on all of the symptoms but it’s too much to write here so just know it was a very bad time.
January 18th- GI appointment day.
Oof. I always know going into these appointments I’m going to get hit with information fast and hard so I try to have nothing else to do the rest of the day so I can go home and mentally process it (which usually means crying).
I walk in and get told, “your liver enzymes are 6 times the max limit which is very abnormal because people on TPN are usually only about 2 times the max. If we can’t figure out what’s causing it, then it means it’s the TPN and we need to remove it and put in enteral feeding.”
I responded, “wait, can I think about this? I just need some time to process this all and then at the next appointment we can talk about it.”
They said, “No, you don’t have time. This would need to be done in April by the latest.”
I said, “What? But I need time.”
And they dropped a huge bomb by saying, “It’s that or you die.”
Hope you enjoyed that cliffhanger!! Read what happens next in the story titled, “Finding the Limits,” ;-).
New Year, New Tubing
I had been informed by my supply company that there was a national shortage of the type of tubing I had previously been using since I got my PICC back in August. It was a type of tubing that was connected to a CADD Solis Pump which I always describe as the Apple product in terms of central line pumps.
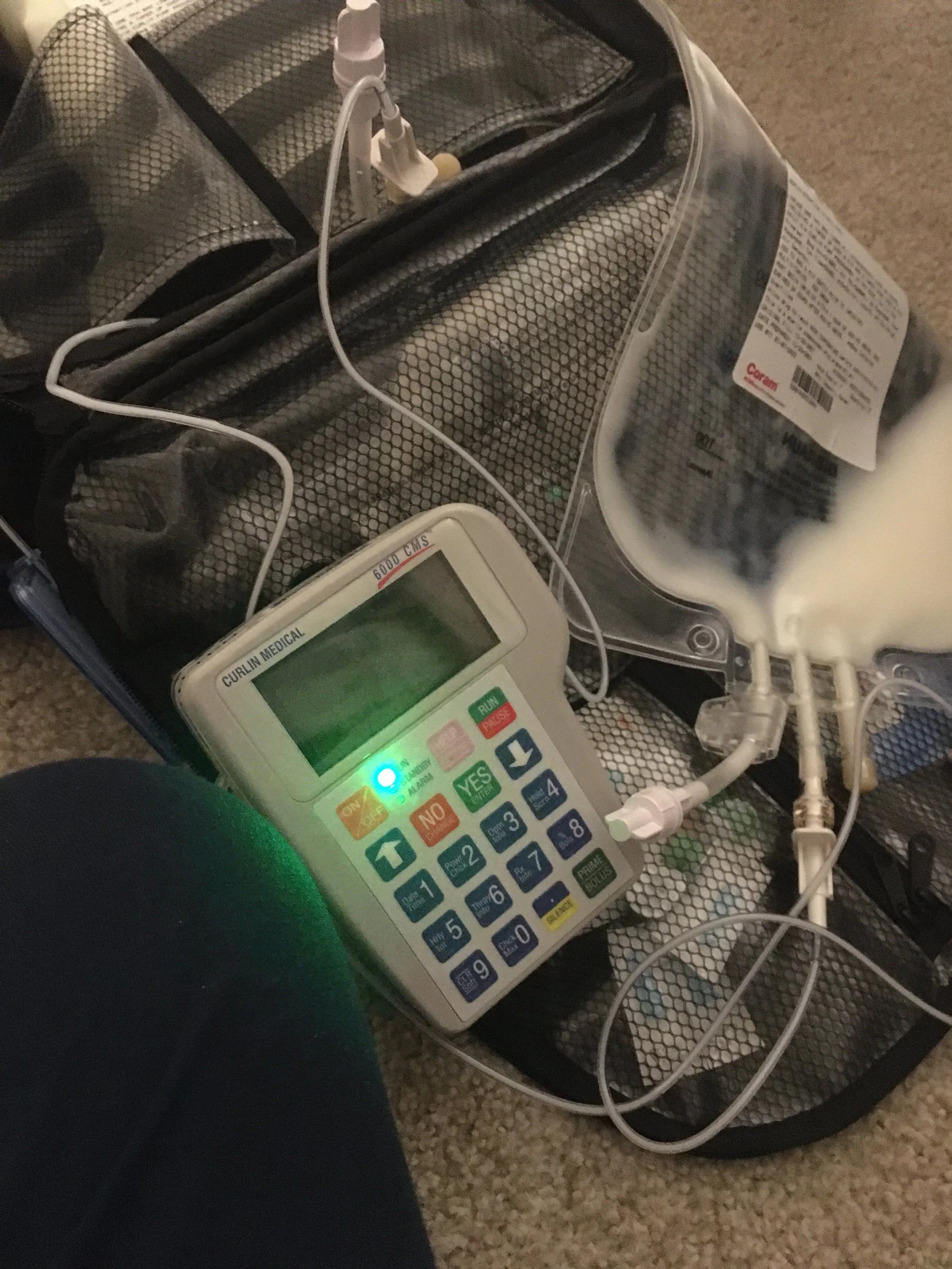
On New Year’s Eve I had been sent the new tubing and new pump (since this tubing only worked with a different pump) and I was so bummed to have to switch. The pump itself was the pumps they used in the 80’s. It was so clunky and would alarm even if you removed the batteries from it!! -You can imagine my surprise when this happened!
The tubing was so thin, and the tube was really short compared to my other one. I have a photo below of my old tubing and how I could reach my bedroom door with my backpack on my IV pole. Now with the new tubing, I only had enough excess to be able to stand up with the bag directly below me.
This took a surprising amount of time for me to get used to because my spatial awareness had adapted since August to the length of the other tube. Also, my TPN change time became longer with the new pump as well. The new pump was weirdly shaped too so it didn’t fit in my backpack properly like the old slim one used to (there was a pocket it used to fit into).
Since the new pump was such an old model, I decided to name it “Gertrude”. I felt it was appropriate, but I wasn’t ready to say goodbye to my nice pump “Steve” yet.
So, I made a plan.
I saved the remaining CADD Solis tubing so when I started back at school in the spring, I had a familiar tube that I felt safe and at home with, in order to give me some comfort among the scariness of starting back at school.
So, in the interim, since I didn’t have enough old tubing to last me through the month, I switched to Gertrude and the MOOG tubing.
On New Year’s Eve I had gotten a new nightstand to help reorganize my room and make it look closer to the “non-medical” room it used to be a year ago.
My roommate, dad and I watched the New York ball drop on TV and enjoyed watching the fireworks through the apartment window.
Unfortunately, among watching the fireworks, my body was having severe pain for some reason, and I had considered taking my oxycodone multiple times but didn’t end up doing so.
January 1st, I rained in the new year in severe abdominal pain with severe swelling and diarrhea!
*Insert a sarcastic “yay” here ;-)*
My pain and nausea just continued throughout the day into the evening, and I just generally felt awful.
On January 2nd I woke up in the late afternoon (body needed to sleep all day I guess) and was able to shower but I was so fatigued.
I was having more esophagus spasms and had more consistent difficulty with swallowing my pills in the evening and in the mornings, so I began taking my muscle relaxer beforehand to drop my pills down in order to swallow them.
This actually helped so much and relieved a lot of pain (since my pills would usually take 2-3 hours to drop all the way down).
January 3rd, I began the first day for the high dose Ibuprofen trial that my GI doctor wanted me to do to see if I had costochondritis. I had waited a while to do this trial since I was so concerned about taking NSAIDs as a person with severe GI issues.
On January 4th I went to see a dentist-first time in over a year (yikes). It was interesting to say the least….
I was explaining to the dentist that I didn’t have the chance to care for my teeth very much because I was debilitated by my illness and was very much focused on the “not dying part”. They seemed uninterested in any of that and were upset that my gums were inflamed.
Other than that though, teeth were doing pretty great! - I take that as a win!!!
I was given a medication for gingivitis and walked home with my mouth literally all bloody and scraped (which made sense because it had been so long since a dentist, but it hurt quite a bit).
I was slowly beginning to get used to changing my TPN on my own with the new tubing and pump which was really great because my dad was set to leave in a couple weeks.
School was starting up soon and we had made a plan that when it started, he’d go back to Texas, and I’d go back to being on my own (since I MISSED MY INDEPENDENCE SO MUCHHH).
The most annoying symptom that was affecting me so much as of late was the esophagus pain and spasms. It was waking me up from sleep and just causing so many problems.
I could only take up to 2 of my muscle relaxers a day which I reserved for the times I had to swallow my pills so the rest of the day I was left to fend for myself.
January 7th, I had a morning virtual meeting for the show I was working on in the spring and I had overslept my alarm. I woke up at the EXACT time the meeting was starting so I leapt out of bed and ran to my computer to join the meeting.
From racing to get up out of bed, I created a dry heaving fit.
I joined the meeting with my camera off and then messaged that I had a medical emergency because I then had to sprint to the bathroom to continue dry heaving (since I thought I was going to throw up).
That evening I was feeling meh (better ish) and I was happy to have my last ibuprofen for the Ibuprofen trial!!!
YAY!!!!
And the results? - You guessed it! - It did absolutely nothing!
As I had already expected (which was why I didn’t want to do the trial, and other doctors of mine also didn’t want me to do the trial….) but I was glad to have my GI doctor stop nagging me about it because I was stuck with them not wanting to do anything else in my care until I did this.
On January 9th I went to an art store with my dad to pick up some school supplies for one of my classes which was set to start tomorrow!!
It was a pretty relaxing day, and I watched a very beautiful and realistic documentary on Netflix about chronic illness (specifically chronic fatigue syndrome also known as M.E.) called “Unrest” with my dad. We both reflected a lot watching it and could relate so much even though I don’t have M.E. It was more about the connections of the debilitating aspects, the clinical diagnosis aspect, and the social aspect that relates to many.
I was excited and nervous to start school the next day since it had been so long since I had taken classes.
The good thing was the first 2 weeks of school were virtual, so I didn’t have to go in person quite yet.
Read how Emma’s in-person classes go in, “Liver Disease, Anemia and Ready for School!”
Vaccines On Top of Illness
The day after Christmas our family continued zooming each other on the TV because I had gifted my mom an escape room box that we all spent time working through together.
It was a lot of fun and reminded us all of the times we used to play board games after dinner when we used to all be living together.
I spent time doing some stamp making since one of my roommates had gifted me a stamp making kit. I enjoyed being able to spend my day doing more crafts since stopping eating (per my doctor’s recommendation) was making me begin to feel so much better and kept me from being immobilized again.
On December 27th I decided to clean my room and reorganize it a bit since I had been feeling better but unfortunately, I once again overestimated my energy and had tremors afterwards.
I had also gotten lab results that were published to my portal, but they were from a month ago (November 30th). The lab results said that I was anemic.
AHH YESS, the thing my dad and I had been fighting to explain to my doctors for months…..
The thing that sucked was I STILL wasn’t able to move up my infusion in January, but we thought it was fine since it would be the following month. We also figured that the anemia was contributing to a lot of my weird fatigue and lightheadedness symptoms.
On December 28th I went with my dad to the hospital to get my cervical spine MRI done. It went well (which was good because I had to call in advance to plan ahead for a private room to disconnect my TPN as soon as I went into the machine). I wasn’t super symptomatic being disconnected which was good, and the MRI took about 15 minutes.
On December 29th my dad and I both went to the hospital to get our next COVID vaccine booster since my doctor had cleared me and said I was now able to get the 3rd booster vaccine.
I knew that in the evening I was going to get allll of the symptoms because I am the queen of side effects. And surely enough, that evening I had a headache, dry heaving, vomiting, fever, chills, muscle aches, etc.
I was stuck in bed again because of how crappy the side effects made me feel.
That evening I had also gotten the results from my cervical spine MRI which had showed some mild spondylosis on my c4-c5 and c5-c6. It didn’t seem like much or anything particularly relevant so I was not very concerned and had to wait until my next appointment anyways to hear my doctor’s thoughts.
December 30th I still had a fever and was still vomiting so I just tried to rest as much as I could. The fever never went above 102 so I wasn’t concerned health-wise.
I was feeling ready for the vaccine symptoms to be over and to celebrate the upcoming new year!
Read about Emma’s New year’s in the story, “New Year, New Tubing”.
Happy Holidays TPN!
Entering into December was a much smoother surgery recovery period because I had my best friends who also happened to be my roommates at the time and my dad there. Everyone got along so well, and it was such a wonderful, unexpected result.
My roommates and my dad had planned to go and buy a Christmas tree together and unfortunately, I was still too sick to go with them. They brought the items home, and we all decorated the tree and the apartment together.
We spent the evening laughing, singing Christmas songs together and watching the soccer match together. My dad is really into soccer, and everyone would make their dinners and then we’d all find our spots on the couch and watch the match together every night.
I am forever grateful for these friends and the fact that they made such a difficult time have such lovely and unforgettable moments. We spent so many nights all talking together for hours (with my dad- shocking right??) and it made those 7 months together feel supported.
The first week of December I was still having some issues with tremors and my hands would sometimes get stuck holding things. But the few tremors I had since being on 24hr TPN, were much more comfortable because I’d take my medication early on to try and shorten the amount of time they occurred for. My best friend would often lay beside me and would talk to comfort me and make them less frightening.
My friend would lie with me in bed all the time and during my flares would hold my hand or hug me when I was crying. They gave the absolute best support and made it feel like I wasn’t going through it alone.
I was still trying to figure out how to have my central line tubes organized because it was super long (the extension of the lumens) and the weight of it caused pain. I tried multiple different methods of clipping it up with tubie clips and catheter covers to try and help offset the weight.
I was super excited for the holiday season because I had already picked out my gifts for everyone and everyone in the apartment was throwing an early Christmas before my roommates left to spend it with their families. I absolutely love wrapping gifts so I couldn’t wait to get on that.
On December 6th I had a follow-up appointment with my primary care physician following the surgery. It went great and was a very routine visit.
I went to my old workplace to visit my boss and to pick up some nice wrapping paper with my best friend. I got home and wrapped gifts in my room (secretly so they couldn’t see their gifts). I accidentally overused my energy and my blood sugar dropped causing me to have a neck tremor attack that evening. I struggled a lot on how to gauge my energy and how to spend it.
-I will say though, my gift-wrapping skills… they looked AMAZING -
I kept running into issues where I kept overusing my energy thinking it wouldn’t cause problems later. I would walk a little bit outside to get gifts with my dad and it would cause large fatigue issues for not only that day but following days too.
On December 8th my physical therapist figured out what was causing my hands to get stuck grasping things. It was an endurance gripping issue where my thumb joint on my right hand would swell when grasping something for 10 seconds and cause the center of my palm to swell also and make me unable to release my hand.
I also had a virtual meeting that day for the show I was supposed to work in the spring at my school and I was really excited for it. Unfortunately, after the meeting I had another neck tremor attack.
On December 9th I tried out a new medication called Propranolol which was meant to help with my POTS symptoms, but it ended up making me more symptomatic and my blood pressure was really low and making me very dizzy.
On December 10th I took a regular shower for the first time with the Hickman. It was a much easier prep in terms of covering it with the shower seals my supply company had given me, but I was so scared it was going to get wet. My nurse had taught me to put a paper towel on top of the Hickman and then to put the shower seals on top so if any water happened to get in, it’d get absorbed by the paper towel. It luckily didn’t get wet, but the fear was definitely there.
December 12th my dad, my roommates and I all headed out to the Seaport market in the evening to walk around which was super fun and the first time I had been out and felt like a human being in MONTHS.
December 13th my nurse had me try out grip locks which was a medical dressing with Velcro to help hold extra tubing. It was super helpful and offset the weight of the line.
December 14th, we had my apartment’s early Christmas which was so much fun, and everyone got each other such thoughtful gifts. We played games all throughout the evening and had lots of laughs.
My best friend even got us all matching shirts of a phrase my dad often said, and we even named our group chat after it. We took some funny photos of us, and all wore the shirts the rest of the day.
December 15th, I walked for the first time to my physical therapy appointment alone!! HOORAY!! It was also a bit of a sad day because I had to say goodbye to one of my best friends who was moving out to go to a college in a different state.
Most of the days I was still having all of my usual symptoms but was able to still do other things throughout the day making it much more livable.
December 18th my dad and I started touring apartments in Boston and had to keep in mind all these new things that the apartment needed to have in order for me to be safe with my illness. I cover more of what things we looked out for in the Advice & Thoughts article titled “Apartment Hunting for the Chronically Ill”.
December 20th, I went to see my autonomic neurologist to go over the latest lab results that had come back weird. My immunoglobulin M and human growth hormone were both elevated, so we wanted to redo them to make sure it wasn’t an error. They also ordered an MRI of my cervical spine to see if that could be related to my tremors. I was also reduced down from 60mg to a 10mg Propranolol pill and was also starting a sodium retention pill to help with symptoms too.
My biweekly labs that my visiting nurse had been doing was moved to monthly which was an awesome sign! I also got my lab results that evening from the blood tests I did at the doctor’s and the human growth hormone came back fine but the immunoglobulin M was still coming back elevated.
December 21st I was feeling super sick for no identifiable reason, and I had been up most of the night from pain. I had hives from abdominal pain and swelling and was dry heaving a lot most of the day and evening.
December 23rd I was taking a shower and noticed through the shower seal stickers on my Hickman, that some of the paper towel was getting wet. I SPRINTED out and immediately started drying the area and peeling off the sticker. I had no idea how the water got in and just kept nervously HOPING that I didn’t just cause a line infection.
December 25th, Christmas!!!
I had wrapped and mailed my gifts to my mom and brother in Texas, and they had mailed their gifts to my dad and I in Boston. We set up a zoom on my living room TV and spent the day “together”. It was really nice, but my energy depleted so quickly that I had to have my dad bring me my gifts and help unwrap them as I lied down on the floor.
Overall though, it was a wonderful Christmas and through the use of technology, we truly did all feel like we were together.
Read about how Emma’s holiday season continues in, “Vaccines On Top of Illness”.
Central Line Surgery!
*Content Warning: Images of surgical site, blood, and bruising at the bottom of article.*
The weeks leading up to the central line surgery I had been preparing myself mentally to see a much more visible and overt medical device on my chest. The PICC was definitely something I had to get used to, but it was always hidden by clothing and my PICC sleeve. Even I didn’t see the site much because of it, but with the central line, it would be in my peripheral always and would be seen if I wore anything that wasn’t a crewneck or turtleneck.
My nurse had also told me to make sure I voiced to the surgeon the ideal placement of the line. The reason this was so important, is because they don’t want anything rubbing against the line and we wanted to make sure the line wouldn’t be under where my backpack strap would need to go. The issue is that it’s something to keep in mind, but it’s entirely dependent on your body and where your veins are located within your body type.
On November 30th, 2021, I woke up at 6:35 a.m. feeling a nervous energy for the surgery ahead. My dad and I arrived at the hospital at 7 a.m. and ended up getting lost trying to find where the waiting room/area the surgery was going to be done. Luckily, my surgery time got moved back to 8 a.m. so we had extra time to find the space.
We finally found the area where we were supposed to be, and it was then that I realized I was getting surgery done in the cardiovascular center (which I guess makes sense, but I thought it was going to be done in a regular operating room or like the interventional radiology center where I got my PICC replaced).
The waiting room was super small, but I waited with my dad trying to get my mind and body ready as if I was about to play in a sports competition.
The nurse came into the waiting room and got my dad’s contact information. My dad said goodbye as I walked down the hallway back into the prep room. I changed into a gown (which was always weird because my tubing would run down the inside of my gown because to have it run outside of my arm, I’d have to disconnect it and reconnect it through the sleeve-just PICC clothes-changing problems).
I was moved into the hallway before the operating room and I was handed lots of forms to sign and told a lot of information about the procedure. I made sure I was getting anesthesia (because it’s INSANE to me that the standard for this procedure is to do it awake. WHO would want to be AWAKE as someone cuts into your chest and shoves a tube into your heart?!!!). I was SOO thankful to have learned earlier on that I could request these procedures with anesthesia because otherwise I can’t imagine how traumatic this would’ve been.
One of the nurses came by to start and IV and instead of doing it in my arm they tried putting one into the vein below my thumb (*insert queasy face). Ohh how that hurt….
It didn’t work because they couldn’t get the vein so they kept repoking it and trying to reposition and I was focusing so hard to maintain my composure. They stuck a bandaid on it and then put in a regular IV on my forearm.
I also mentioned to the nurses and prep team about the location of the central line (which was going to be a Hickman line-just the brand name of the line I got put in) and they mentioned they’d try their best and would mention it to the surgeons.
After waiting a bit in the prep bed, I was rolled into the operating room. The room was smaller than the IR room I had been in before, but the equipment and table looked similar. There were so many people in the room all preparing things and it was a bit hectic.
I scooted onto the table and sat up trying to help the doctors disconnect my TPN as they asked me questions (and some were trying to get me to lie down). Through the glass window I could see the whole other plethora of doctors whose job was to monitor my vitals and monitor signs.
I thought I was going to have to be awake for the removal of the PICC since they usually have you hold your breath as they pull out the last 15cm of the line in order to not have an air embolism. Luckily, they did the removal while I was under anesthesia.
I remember laying down as the anesthesiologist was counting off and I was slowly drifting off to sleep.
At around 11:40 a.m. I woke up in the recovery center and felt so nauseous (always happens to me with anesthesia). I felt a very deep pain in my chest and couldn’t move my upper body or right shoulder without immense pain. My neck had been taped (it was a pressure dressing) and it was preventing me from being able to hold my head straight.
I was basically an exhausted zombie and looked awful.
A nurse caught on and gave me a stuffed animal to cheer me up- which was actually really sweet of them.
I remained in the recovery room for 30 minutes for monitoring and my dad was invited in to see me. We were given a folder with limited information on the procedure and were discharged.
We took the wheelchair on the way home at around 12:30pm and I immediately went to sleep when I got to my bed.
I woke up at 2:41pm and had a popsicle and then felt so nauseous. I had help from my dad to make it to the bathroom to pee, but I was just dealing with so much pain that day that I was trying my best to keep it together.
Continued sleeping the rest of the day and felt better-ish towards the evening.
On December 1st (the following day) I was crying every time I moved from the pain. I mostly rested in bed and tried not to move.
I had a really tough time trying to figure out the best method to sleep and not get my tubes pulled because the line was really heavy and the weight of the tubing would pull causing more pain. I did a lot of trial and error and still couldn’t find the method that worked best even for during the day.
The following three days I was usually up all night from pain and slept all day.
The site was bleeding more over the few days just from the minimal movements I was doing, and my neck was still taped up funny. I hadn’t showered in a while either since I could barely get out of bed.
It was a rough recovery but definitely worth it in the long run.
Read how Emma’s month continues in, “Happy Holidays TPN!”
Happy Thanksgiving! Leave An Empty Plate!
The weekend before, 48 hours before, and the day before, I had to call TSA to prep them for my travels. I was really nervous to travel because I was afraid they’d turn us away or we’d miss a flight because of the TPN.
I had also packed with me a small folder of medical packets and letters from my doctors in case I ended up in the ER during my visit in Austin or if any of the airports had any questions.
On November 23rd my dad and I woke up at 2:34a.m. and headed for the airport at 3:30a.m. We had to book an early flight because it needed to be at a time that I didn’t need to start thawing my new bag of TPN, and early enough that it didn’t hit my change time.
In Boston we went up to the TSA guards and let them know I wanted a Passenger Support Specialist (PSS) but they didn’t have one in the airport at the time. They just had me go through the x-ray with my backpack and then swabbed me for drug tests at the other side. It was very simple, and they just let us through.
To board the plane, we were under the first to board since we had to fit my medical bags in the overhead bins. I explained to the flight attendants about my condition and that my bag needed to stay in my lap since it could slide under my seat accidentally and rip out my PICC.
Everything went pretty smoothly, and they didn’t even ask to see my pump documentation which made things really easy (read more on “Traveling with TPN” in my ‘Advice & Thoughts’ blog section).
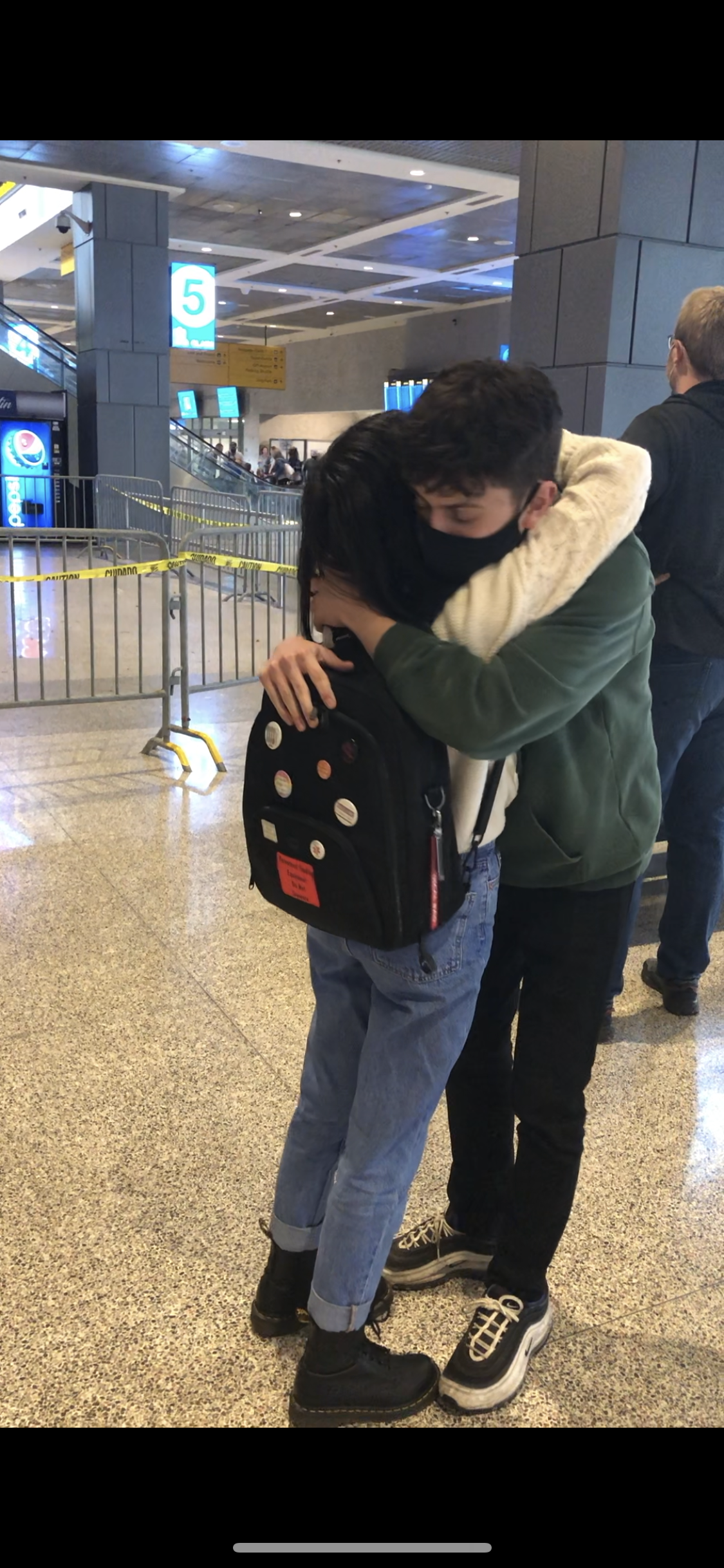
I arrived in Austin at 11:30a.m. (CST) and I was so excited to see my brother. He was arriving in from a flight coming from California an hour later so my dad and I waited in the airport.
My brother’s flight finally landed, and I got to see him for the first time in a year. It was so crazy to see him especially with the TPN and everything now.
We took a Lyft home and got to see our dog and I immediately fell asleep on the couch from the busy day.
I had set all these alarms on my phone for my TPN change time since there was a time difference, and my pump would end and hour earlier.
My carry-on makeshift ice bag worked out and when I had arrived earlier on in the day, the ice we brought was still nice and cold along with the TPN. My mom had prepped space in the fridge in advance, so my dad loaded them in.
On Thanksgiving, I had a great day spending time with my immediate family. I was feeling pretty nauseous that day but luckily had all of my medications with me to help with my symptoms. I had also taken some Carafate since the evening prior I had some soup (I had my mom order the same brand I had been eating in Boston).
It was a bit tough not being able to eat anything during Thanksgiving but luckily my family never cooked much anyways since it was normally just the four of us. I think also me being pretty nauseous all day helped curb any potential hunger cravings I might’ve had.
Amongst all of the family fun, I forgot to take out my TPN to thaw so when I reconnected in the evening I was shivering. The best way I can describe why it has to thaw is, it’s like ice running through your veins. Chilling and sometimes painful.
On November 26th my family and I went to an outdoor shopping mall for some of the day to walk around and then in the evening we had a gingerbread house competition. We watched the “Great British Baking Show” every night, so we wanted to put our viewer skills to the test. After we were done, I made a gingerbread village for our houses to reside in.
November 27th, I was woken up from esophagus spasms in the morning and continued having bad spasms for the rest of the day. Took lots of nausea medication and muscle relaxers. Spent more of the day with the family enjoying our time together and playing board games.
That evening I hugged my brother tight knowing that I was not going to travel to Austin again because of how much prep and stress went into traveling. My mom and I said a temporary goodbye since we knew she would be coming to see me in Boston in April to help me move apartments.
My dad and I were ready to head back to Boston with a day of rest before my surgery.
On November 28th, TSA Cares Austin called me to prep a PSS to meet me at the airport. I had to call a couple times since they requested me to so we could meet up inside.
The airport TSA line was all the way out the door at 5 a.m.! It was insane!
I found my PSS and they were so incredibly kind. They brought us all the way ahead of the line, but I was stuck being checked for so long!!
They seemed to be really confused with the TPN and kept asking to test the liquid inside of the TPN bag. I was really hyper focused because there were 4 TSA agents checking all my bags at the same time, so I was trying to make sure no one was poking the bags making them unsterile. At the same time of watching all of them, I was being checked and also asked questions at the same time while people in the TSA line were staring at me.
It was definitely tough, and I was trying to not feel embarrassed while they examined my PICC site and bags.
They took out all of my TPN bags out of our makeshift ice “cooler” suitcase and swabbed the outside of each one.
When they were all done, my dad and I had so much to put away.
When we got to the plane, we alerted the gate agent we would be boarding with the disability line. I got on the plane and explained to the flight attendants the same thing I told the ones in Boston.
However, they were very confused, and we ended up taking off slightly late because of how much hassle the TPN bag was! They kept getting flight attendants and then going to the front of the plane and then coming back to ask me more questions.
It was really taxing, and I wanted to just be home and resting.
When I finally made it back to Boston, I took a 5-hour nap. I was so exhausted from just the energy it took to be alert and answer everyone’s questions. It also took so much to ignore my symptoms to focus on the day so my body just kind of collapsed.
That evening my friend and her mom came over and we played an escape room box the whole evening with everyone in my apartment and it was so much fun. We all learned we aren’t great at escape rooms :-).
On November 29th, I spent the day resting in bed watching movies to try and distract myself from nerves about the surgery the next day. My nurse came by and changed my last dressing with my PICC line.
Off to bed I went, feeling ready-ish for the surgery the next day.
Read about the central line surgery in the article, “Central Line Surgery!”
Searching For the ‘Other’ Problems
The days following November 12th, I continued to be on the phone sorting out travel stuff and gave my mom a list of medical supplies to buy to have at the house (IV pole, sharps container, etc.)
I also began prep packing to see how everything would fit since we were told my supplies couldn’t be shipped to Texas since they didn’t have my supply company where I lived. Therefore, this meant I had to have a minimum of 3 carry-on bags carrying my medical supplies (not including a regular carry-on and my dad’s bags).
By mid-November, I was able to walk around more (switched out my ambulatory wheelchair pin for a “please offer me a seat” pin) but was still lightheaded after walking for a bit so I still needed to take Lyft’s everywhere and needed to sit down once I made it to my destination.
On November 15th I headed to a new hospital to look into the autonomic issues and other weird body issues (like the tremors and hand locking). The appointment went super well, and the doctor was so kind. Everything they asked they genuinely listened and wanted to look into it. I was sent to the blood lab after where they took 12 tubes of blood! I had to come back the following day to do 2 more tubes because they wanted to send them to Mayo Clinic but they just didn’t have the correct tubes in stock. I had also been given a 24-hour urine sample kit that I needed to complete and bring back.
That evening I received a phone call from a super kind member of my supply company who helped me arrange more for my upcoming travels. They helped me feel a lot calmer and I got a lot of my questions answered.
On the 16th, I got emails from the hospital for my Hickman procedure date and time with a confirmation that I would be under anesthesia, but they had the incorrect dates, so we waited for them to reach out again with and updated schedule.
I went to visit my old boss (from the summer when I was working) and it was super nice getting to see them again, this time with me out of the wheelchair.
In the evening I received a phone call with the finalized central line surgery date which was November 30th at 8 a.m.
I had also gotten some of my lab results back from the hospital I visited the other day and a couple results were unusual but nothing of concern, so I notated them in my binder and knew I’d get more answers about it at my next appointment.
November 17th, I noticed that after physical therapy my injured toe would swell up after activity and walking and then shrink back down when I elevated it and rested.
From the 17th-18th the soup broth I had been so consistently taking for many months began to irritate my stomach and cause hives, pain, etc. I had restarted the Carafate to see if it would help my symptoms, but it didn’t.
I also completed my 24-hour urine test on the 18th and headed back to the hospital to drop it off and complete those last 2 blood tests.
Also, through this time, I was waking up every morning at around 8am-10am racing to the bathroom to pee. Usually at this time every 2 hours I’d have to pee with the amount of fluid being consistently pumped into my body. Sleeping meant I wouldn’t be able to pee for many hours, so I’d be woken up from sleep in the morning to go do so.
I continued prepping packing ideas and how we were going to fill a carry-on with ice to hold my TPN (we were going to get a cooler, but it wouldn’t arrive in time, so we needed the next best thing).
On November 22nd, I had another GI appointment just as a formality before the surgery. It was with the nurse practitioner and was very bureaucratical. My dad and I did try to get in (for the millionth time) that we wanted my iron infusion to be moved closer since we both believed I was anemic and hadn’t been getting iron for very long.
-This didn’t work. Eh, we tried.
Finally, November 23rd arrived!! Travel day!!
Read how Emma’s Thanksgiving went in, “Happy Thanksgiving! Leave An Empty Plate!”
Big Strides! Able to Walk!
After the mashed potato flare ended, I was back out of the wheelchair and walking again (which I am very fortunate to have been the case).
I was excited because I was headed to my school on October 30th to watch the production that I had been assigned, but wasn’t able to finish working on since I took a medical leave of absence from school.
I had been planning what I was going to wear since I didn’t want to have to wear my sweatpants. I also wasn’t sure yet if I was going to take the wheelchair or not. I found an outfit I had liked but the problem was I had still been to bloated to fit into the pants, so I put on a scarf overtop like a shawl to cover the fact that the pants were unzipped.
On October 30th, I decided I was going to walk there (took a Lyft to get there and then walked inside). I was so excited and also a bit sad seeing all of my friends having fun and getting to work on shows. It was a beautiful production, and I was so glad to have been feeling well enough that day to have seen it.
On Halloween I had my roommate and my other best friend come over and we played games with my dad all evening. It was super fun but from laughing I started swelling up a bit from my stomach being moved.
On November 2nd I had my dad start teaching me how to put in the vitamins in for my own TPN bags. Since my goal was now to try to go to school in the spring, I wanted to start learning how to be self-sufficient with my medical supplies.
I also began more routinely showering and was able to do it on my own. The prep for my showers also was cutting down to 15 minutes to get ready (which was way better than the 30min-1hr it took before).
On November 3rd I began having a good day in physical therapy since I was able to walk to and from the appointment. Later during the day, I received a phone call from my GI doctor that was surprising. I put the phone on speaker and walked into my living room with my dad and my roommate to listen in. They were yelling at me expressing their frustration with my case. They were upset that my case wasn’t progressing, and that they were not as kept in the loop as my primary doctor. They were also upset that I wasn’t trying the NSAIDs for the costochondritis at the moment and even said I should switch to a different doctor. I had also mentioned that I was planning on going to Texas for a few days for Thanksgiving which they weren’t thrilled about either (because we were trying to see if we could fit the central line procedure before).
On the phone I calmed them down by saying, “I understand this case is frustrating, believe me, as the patient, I get it.” I also said I didn’t want a new doctor (because this was the only one in the state that at the present moment, that was leaving me on TPN). So, I was absolutely going to do as much as I could to keep them.
After they hung up, my roommate and dad’s jaws were dropped. They were so shocked at the tone from my doctor, and I was so surprised I was having to calm them down.
I wrote a follow-up note to them clearing up any “lost in translation” items which I have included a photo of below with of course redacted information.
The next couple days, we further solidified plans for traveling to Texas for Thanksgiving and bought the tickets. I would be there for 5 days. I was super excited to get to see my brother who I hadn’t seen in a year. The stressful part of everything is the prep to fly was going to take weeks to contact the airports, my medical supply companies, etc!
We also decided to extend the central line procedure to be done in December since I didn’t want to fly to Texas in pain, and if there were any complications I wouldn’t have my doctors, etc.
I continued having my usual esophagus spasms and abdominal pain over the weeks but generally had much more energy to be able to handle it all with the TPN.
November 5th was the first day I began having hunger issues. I was starving and my stomach was grumbling, and it made me reconsider breaking the “fast”. It took a lot of self-will, but I managed to not crack and tried to do something else to distract myself.
Unfortunately, that “hunger craving” sensation hasn’t left me and only got much harder to hold at bay.
I understood why Gastroparesis’ slogan is “starving for a cure”.
On November 6th I went shopping for the first time in 4 months. I had gotten some new clothes for my trip and they fit better with my new swollen and bloated stomach that was here to stay.
I also had gotten some Thanksgiving tubie clips and catheter covers for my trip.
On November 8th, I spent the whole morning calling TSA and prescheduling my trip. I requested a Passenger Support Specialist (PSS) to help me get through the TSA line. *In my “Advice & Thoughts” blog tab, I have a whole article on how to fly with TPN (“Traveling With TPN”).
I also received a phone call response from my GI doctor in response to my email which was once again a bit heated. They wanted to urgently do the central line procedure and said it was extremely dangerous that I was waiting. I explained that I didn’t even know I needed the central line until my dad accidentally brought it up in an appointment. If he hadn’t, they wouldn’t have even realized how long I had been on the PICC. I remained calm and tried to get things cleared up so I could get the procedure done after Thanksgiving.
I once again sent a follow-up letter since the letters seemed to be comprehended more on their end then when I spoke. This second letter has also been included below.
On November 9th, stress was heightened as I was awaiting phone calls all day. I was on the phone with the airline to find out more travel info and all the documents I needed to bring. I was also on the phone with the airports themselves and once again TSA. I also called the supply company and was on the phone with them. I had heard from my primary that IR (interventional radiology) was going to call for when my Hickman Line was going to be placed. I had been told over email that they were going to place the central line that week, and the phone call was going to tell me when (but then that didn’t end up happening… all very wishy washy).
On November 11th, I worked on the art for my brother’s music albums in bed. In the evening my friend brought their dog over for us to pet sit and my roommates, my dad and I played games and laughed all evening.
On November 13th, I signed up for my classes in the spring. It was surreal but made the goal feel so much closer.
Fun and relaxing times were ahead but first I had to make it through getting all of the medical travel stuff scheduled and arranged!!
Read more of how the month of November went in the article titled, “Searching For the ‘Other’ Problems.”
Uh-Oh I Ate Mashed Potatoes!
After my appointment with my GI specialist, I followed their advice naively instead of thinking of the past and realizing I had already done their food trials (the 3 months I continued eating which only worsened my pain and caused more severe symptoms) and had dire consequences.
On October 20th, the day after the appointment, I looked at the food list my nutritionist had given me and decided to try the mashed potatoes later that day.
I had gone to physical therapy, and it was my last day with my physical therapist since they were moving to work at a different hospital. To make it memorable, I was able to walk up and down the stairs (with assistance) and didn’t need as long a break. It was hard to say goodbye but I’m glad we spent such a great last appointment together.
When I had gotten home, I was feeling really motivated after such a great physical therapy appointment, so I worked on some stage management paperwork for a show I was going to *hopefully* do in the spring.
At 3:30pm that day, I heated up a mashed potato cup and ate a couple spoons of the mashed potatoes.
At 8:30pm all hell broke loose. Little did I know that these 2 spoonsful would result in a week long flare.
My stomach on my upper left side had swollen out and I began having diarrhea and nausea. It was the time when reality hit me and I realized, “why did I do that?”
I kept doing the same thing over again and expecting different results- AKA the definition of insanity- per my doctor’s requests.
I didn’t sleep much and was woken up multiple times in pain. I had more diarrhea and had lots of dry heaving the next day.
On October 21st my pain just kept escalating and I was just stuck in bed crying since none of my medications were helping with my pain. My dad’s company sent some flowers to me (unknown to me or my dad) and it was really nice to have some extra support on such a tough day.
I sent out that evening a 2 paged letter to my medical team expressing my disappointment in them not listening to me and having me do these “trials” and it failing, for them to want me to just “try again” while I’m left to suffer through it.
In the letter I expressed how all my work in physical therapy went down the drain just from eating a couple spoons of mashed potatoes because I was immobile again and needed the wheelchair to get up and move around. I requested to have the central line placed since I didn’t want to subject myself to more torture for nothing. I also requested to have my pump time remain at 24 hours and not jump down an hour since I was so symptomatic being off of it. I also told them I wanted to go back to school in the spring. (I have included the letter with redacted identifying words below with the images).
On October 22nd I had a phone call with one of my GI doctors at a different hospital (the ones who were looking into MCAS and Mitochondrial diseases) and it was a very upsetting call. We talked and argued as I was fighting to explain why I needed to remain on TPN and them advising strongly against it. They ended the call saying if I wanted their help on my case, I needed to switch to their plan fully and be put on an NG tube with enteral feeding. I also told them I wanted to go to school in the spring which they were very strongly against. They said if they were me, they’d be doing everything in their power to find out what’s wrong and not waste my time going to school. This frustrated me because they hadn’t been in this journey for as many of the years as I had been. If they had been, I’m sure they’d have very different thoughts.
Emotionally during this time, it was so challenging as I began for the first time fighting to have a life and everyone was against me. I knew I wanted to go to school in the spring so everything I did onward was to accomplish that goal.
On October 23rd I woke up unable to talk or move from pain (because I was still flaring from the mashed potatoes). I had to take my oxycodone so I could make it to the bathroom in the wheelchair to pee.
On October 25th I saw my primary care physician while still in the potatoes flare. They were on my side with everything I wanted to do. IT WAS SO AMAZING! They wanted me to go back to school and they would remain as the only doctor on my side up to my care today. They also at this time gave me the best advice any doctor had ever given me, they said, “stop eating, please stop eating. We don’t know how much damage this could be causing to your body.” They also were ‘for’ me getting the central line and I told them that the only way I’d do it, is if I was put under anesthesia for the procedure since I REFUSED to be awake as they cut into my chest and neck for the line. They agreed.
On October 27th, the day the flare was ending, I walked to my physical therapy office which I was super proud about. Afterwards I had some pain in my abdomen and got hives again.
I received a phone call from my dietician/nutritionist who told me they agreed with my plan from my letter. They said that whenever I was comfortable, I could disconnect for like 10 minutes whenever I needed to shower.
I also had ordered a new TPN backpack which I received that day and sewed on an iron on label that said “parenteral feeding equipment do not separate” for any future hospital visits so people stopped yanking away the backpack, pulling me with it. I also resewed the inside to be able to fit my massive 2 liter TPN bags.
That evening I was putting together more items for the medical binder and was reading my barium swallow report. It was then that I noticed the report had incorrect information on it that had been affecting my care :-( . It said that I had swallowed the pill at the end and that they “saw it reach my stomach”. Huh, WEIRD considering I never swallowed the pill, guess I have teleportation powers.
I then called the hospital who then had to call all these people and the witness said that I never swallowed the pill. They then sent out in the following days an addendum piece that said I didn’t swallow the pill.
It’s a good thing I got a new portal when I was an inpatient to be able to see this document because otherwise, I wouldn’t have been able to read it.
Lesson from this- READ YOUR REPORTS CLOSELY!
Read what happens next in, “Big Strides! Able to Walk!”
Which Came First, The Chicken or The Egg?
My GI appointment on October 19th, 2021, started the largest debate that all my doctors still argue today which is, “did the Gastroparesis happen before or after starting TPN?”
I rolled to my appointment with my dad, and we took turns with me sometimes wheeling myself until I got tired and needed my dad to take over. The appointment was going to have both my GI doctor and dietician/nutritionist present.
This was the first time I was going to have an in-person appointment with this new doctor I had been assigned, who also was the head of the department of that hospital.
They first mentioned the results from the Gastric Emptying Study. They said it showed severe gastric delay but that they think it isn’t as severe as it was showing. They said that not being able to eat and being on TPN for so long likely was skewing the results of the test and I probably only had mild delay. They said I might’ve had some delay prior to TPN but not likely.
So, HERE’S the issue with this-
Gastroparesis could explain a lot of my symptoms and why I had such difficulty as I continued eating over time. The big problem is because they scheduled the test so far out from when I started TPN, they could be misattributing it to the TPN. My dad and I both discussed that my doctors would be handling things very differently had this test showed the same results and I had taken it the week I was discharged.
Every doctor I’ve seen believes a different timeline and I believe I did have gastroparesis before and that it likely mildly worsened with starting TPN. The other fact that people kept forgetting is I was still having things move through my digestive system daily. I had tons of pills that I had to take every day throughout the day that I had with water. I also had soup occasionally (used to be daily but stopped it after the GES test because of the flare). So, this disproved the statement as well.
They said they wanted to do another endoscopy and colonoscopy in April to look into some of the things that the other hospital had suggested.
During the physical exam they saw how inflamed my upper left abdomen was and thought it was rib cartilage inflammation. They diagnosed me with costochondritis and wanted me to up my dosage of Tylenol and then trial a high dose regiment of Ibuprofen (which I was cautious about trialing with all of my GI issues).
My dietician and GI doctor wanted me to trial pureed foods over the following week and gave me a diet plan to begin. On the list were things like mashed potatoes, apple sauce, and cream of rice.
My GI specialist had asked how many weeks I had been on the PICC line for and when I responded 17, they were shocked. They told me that they normally take patients off of it at 14 weeks and if they still can’t eat, then they’d get switched to a central line.
I was sent home with the information of what to trial eating and that if I couldn’t get my intake up, I’d have to get a central line placed.
They had also wanted to try taking me off of TPN for an hour to try and give my liver a break from constantly filtering the TPN.
Later that day I had my soup broth, but this time had a couple noodles. My stomach hurt but it was fairly tolerable since I had energy to take it. I did have some issues swallowing it but not too bad and I only had like 2 noodles.
Read what happens the following day when Emma trials eating mashed potatoes in, “Uh-Oh, I Ate Mashed Potatoes!”
Adjusting On the Tightrope
Since my eating at this time had gone down a lot, I was up moving around a lot more and was able to do activities during the day.
I was still using the wheelchair and I had gone out with my dad one day to go to Target. On our way back home, we walked through the park, and I rolled on the street parallel to my college campus.
I had a really tough time because I realized through everything how much I care about how I present myself. Basically, I care about presenting myself in a certain manner publicly and my illness wasn’t allowing me to. I always had my glasses on since procedures and me sleeping all the time meant I couldn’t have my contacts in. I was wearing sweatpants because my stomach was so swollen, I didn’t fit into any of my clothes. I wore loose t-shirts because my stomach was super sensitive to anything touching it. My hair was always pulled back in a ponytail since I couldn’t shower as often and would vomit a lot and needed it out of my face.
That day, I had rolled by someone I knew on campus. I waved at them, but they didn’t recognize me and kept walking past. It was a hard reality that they didn’t recognize me. I did cry after this incident but in the long run it helped me adjust to the fact that I wasn’t the same person that I was before.
For the next few months, I struggled a lot and was frustrated that I wasn’t the old me since I had lost so much of what made my identity. I had begun seeing a therapist a couple weeks prior to help me find out who I was now and how I could deal with that new reality.
My roommate at the time also let me know that they were moving states to transfer to another college. This then allowed me to have a new activity that brought me lots of joy among the days in bed. I built 3D interior design models of what a potential apartment designs could look like for me on my own.
I had never decorated a space for myself since I never knew what I liked, so the time I spent finding out what I wanted the interior to look like, I began starting to rebuild the pieces of my identity.
I spent most days for the next 5 months working on the design.
My dad and I started brainstorming how this was going to work in the more literal sense because we would need to go apartment hunting soon to get ideas before my lease ended in the spring.
A lot more went into apartment hunting this time around since we had to think about all of these things we didn’t need to before. The place has to not have stairs in the entrance and needs to have an elevator for the wheelchair and for stretchers to get in and get me. Is it safe area for me to be living alone in? It has to have laundry in unit since I won’t be able to travel far and get to certain places. Needs to be near a hospital with how frequently I visit there, etc.
My dad and I notated these things and kept it in the back of our minds for when we would start looking later in January.
I enjoyed being able to have more energy and think about these things and was excited to be walking around more in the house without the wheelchair.
In the past my dad and I had many conversations about what my career would look like if I was stuck in the wheelchair, and we had planned out how every avenue would work in case the path steered in any of those directions. It helped me cope a lot to face the reality of everything and keep venturing further to see how life would be down those paths. I’d cry a lot, but it helped to address the scary things when they came so I already knew what to do if they happened instead of keeping it in the back of my mind eating away at me.
Rebuilding myself after being left with very little pieces was the most challenging thing I’ve ever had to do. I had rebuilt myself after the Texas flares, but I had not nearly lost so much of myself as I did this year.
I’m proud to look back and see how far I’ve come but this story is to show a glimpse of the reality of how difficult it is.
In the next story titled, “Which Came First, The Chicken or The Egg?” you can read about the result that left the largest debate in my care to this day.
New Doctors, More Tests & Still No Answers
The days following the emptying study I wrote minimally in my journals due to dealing with the severe pain and being unable to write. Amongst the pain I was still having reactions from the senna (see the story titled, “Tubie Clips & Wheelchair Gear,” for more info) but it was slowly dying down over time.
Back over the summer my mom had scheduled an appointment for me to see a pediatric GI specialist at a hospital that was known to handle rare cases. We kept the appointment to see if they had any ideas.
I had been called a week prior by the hospital with them wanting to drop the case, but I called them back and fought to keep it.
On October 11th my dad and I went to the appointment. It happened to be the same day that Boston was having their “make-up marathon” so we left extra early to be sure we made it on time.
I was having an extremely high pain day and therefore my emotions were on the brink. As my dad helped me into a Lyft, I burst out crying from pain.
As I am with most of my appointments, I was on edge- curious what type of doctor I’d be seeing. I knew they were the head of the department but that isn’t always a good thing.
I saw the doctor and they had the medical team see me as well during the appointment.
They examined me and didn’t want to see the binder (which is fine- I always bring it in case). During the physical exam I cried out since I was already spiking in levels above 10 all day.
The doctor asked me what I wanted out of everything- I had never heard someone ask me this so I didn’t really know how to answer. I started crying because I hadn’t ever heard a doctor express a concern for me as a person before (except for my PCP I had at the time). I said I didn’t want pain anymore but that isn’t my true answer. My more realistic answer in a calmer mindset is: I don’t want to continue having massive flares that leave me bedbound for over half a year.
It was quite awkward crying in front of their team, and I tried to get myself under control again since I didn’t feel safe to cry.
They then expressed their opinions on my case; they said they highly disagreed with me being on TPN and wanted to look at my pain as the illness instead of a symptom. They believed I had multiple undiagnosed issues that were contributing to each other making everything worse. They wanted the nerve entrapment in my abdomen to be handled with cortisteriod injections to reduce my overall pain levels.
-I want to interject here and mention we did inform them that I was told by multiple doctors to never do cortisteroid injections again anywhere due to the severe tissue loss that happened to my foot. They told us we could do Botox injections instead. -
They wanted to send me to the Mayo Clinic to do rehab to get me out of the wheelchair and get me eating again. They said it would be really painful but over time it wouldn’t hurt anymore to eat.
We asked how they knew that, and they said they’d seen tons of cases like me, and I just needed to not be afraid to eat again.
-Okayyyy, let’s take a pause here. I think we all know I have no problem with the psychology behind eating. I’ll eat anyways and if I knew it was going to enable me to eat again, I’d do it. But the fact is, it wouldn’t work. How do I know? Because of the past, it’s happened every time. –
We told them that we hadn’t heard the GES results and asked what they thought. They said they guaranteed the test would come back showing nothing.
Well! Were they entirely wrong!!! (also, why you don’t guarantee things…)
So, we didn’t love this appointment and I knew that everything they were saying I had a response to why things were the way they were.
I was stuck in a wheelchair due to pain and nausea. Alongside this, being in bed made my muscles atrophy over time but I knew I could get the muscles back fairly quick.
The eating was not due to a psychological fear but rather the fact that I knew continuing to eat would worsen symptoms, not make them better.
After my appointment, they requested to drop my case and said I could find better help elsewhere.
The following day I had physical therapy and was informed that my physical therapist that had been with me for almost a year, was leaving to work at another hospital. That day I walked 2 laps in the office without any sitting breaks.
My GES result came in that evening and showed “severe gastric delay” and “prolonged emptying”.
I had also gotten notes back from my neurologist regarding my tremors which they believed could be cervical dystonic tremors (cervical spine).
Lastly, my stool test came back (which again take into account the senna reaction) showed intestinal inflammation with Calprotectin being 59.9 (which isn’t even that high).
Two days later I had an echocardiogram done to make sure that my high heart rate wasn’t because of any physical heart issues. The test went well, my upper left abdomen hurt a bit since for some of the exam they had the ultrasound monitor there. All results came back looking great! My dad said during the test he could see the end of my PICC line bouncing around in my heart from my heartbeat.
On October 15th, I went to my college major’s yearly kickball game to watch on the sidelines. It was tough seeing all my peers in their fall semester but nice to see old friends.
After all of these appointments, I entered into the reality that nothing was coming up next in terms of new tests or big appointments on the horizon. I had to grasp that I finally needed to live in the present since that’s all I was left with during this limbo.
Read the next story, “Adjusting on the Tightrope” to find out how Emma’s life in the new limbo was.
G.E.S. You Are My Nemesis!
So, the test we were supposed to get done the same week that I was released as an inpatient back in August ended up finally happening on October 8th.
I was woken up at 5:15a.m. on October 8th from diarrhea (because of the senna I had taken-read the previous story for more info) and decided to stay awake since my Gastric Emptying Study (GES) started at 7:30 a.m.
My dad and I went to the hospital at 6:40 a.m. and made our way to the GES test wing which was silent in the early hours of the morning.
I was quite nervous for the test, and I had done research prior to know what to expect- I don’t like surprises and like to be prepared going into medical things.
So, the breakdown of the test- GES is a study to measure digestive motility. This means its measuring how fast/slow food and drink is moving through your whole digestive tract to see if you have a motility disorder. This test usually takes a long time since your body has to digest the food. You are given (in the USA) 2 scrambled eggs that contain a radioactive material that they can trace in the x-ray machine, 2 slices of bread, butter (if you want), and 120mL of water. After eating the food you’d be x-rayed multiple times over the hours to see where the food is to determine the speed at which you’re digesting.
So that’s the information I knew about.
I had also been told by many doctors that I’d likely throw up since many people did after eating the eggs.
7:20 a.m. - My dad and I were in the super small waiting room with my wheelchair cramped in the middle and the radiologist came out to explain the exam to me. I suddenly got a lot of information I didn’t know that made me really nervous.
I was informed that I had to finish eating the whole plate in under 5 minutes. If at any time throughout the test I were to vomit, the test would be void. If I didn’t complete the meal in five minutes, the test would be void.
Oooof, that’s a lot of pressure…
I requested gluten free bread and was told I’d be brought back in 10 minutes to start the exam.
In the waiting room I had brought a stress ball that I was squeezing and felt like I was about to compete in the NBA Finals.
7:30 a.m.- Game time. The radiologist wheeled me back as I said goodbye to my dad and put my game face on. I knew in my mind I was going to get that food down come hell or highwater. I knew that this test was the biggest clue and chance of me seeing something wrong, so I needed to complete it for myself and my medical teams.
I am told to sit at a table beside the large x-ray machine as I am explained the food in front of me. There’s 2 scrambled eggs, 2 large gluten free rolls (the radiologist said the kitchen didn’t have gluten free bread slices), butter, and 120mL of water. They pull out their stopwatch and say, “ready, set, GO.”
There I go like a horse off the races, I grab a spoon and begin shoveling the radioactive eggs into my mouth quickly drinking water to get it washed down- of course forgetting I have swallowing issues. I grab one of the bread rolls and begin taking large bites, but the density of the bread slows things down, so I go back to the eggs (since they have the radioactive tool that they need to measure).
I am consistently shoveling food in that at no point is my mouth empty. After 3 bites in I already was gagging. I kept eating anyways.
I begin vomiting into my mouth but swallow it back up because I was NOT about to void this damn test.
Seconds are flying by, and the radiologist re-enters the room and bends beside me showing me the stopwatch and keeps yelling, “hurry up! Hurry!!”
-This was not helpful-
I’m shoveling in food and pouring water down as I’m battling more vomit and swallowing difficulties.
I’m almost crying from the pain and discomfort as the radiologist tells me I’m almost out of time. They said if I can’t finish the meal the test is void and I need to again, “Hurry up!”
-Again, not loving the radiologist at this moment…-
The radiologist comes in and tells me I’m over time and I yell back as I’m chewing, “I haven’t eaten a meal in 3 months! Give me some time, will you? I’m not going to finish the plate so tell me what it is you want eaten!”
-I want to emphasize how extremely short five minutes actually is to complete a meal. I think the only way a person could’ve eaten the meal under time would be to cut the rolls in half, pack it with the scrambled eggs and down the two sandwiches and then chug the water at the end. All things I couldn’t have done at that time-
They watch me as they point at what else I need to eat on the plate. Then they tell me to get up since we’re already behind on the test.
They tell me I need to lie down (which did not help at all with my GERD) and have this large x-ray over the top of me that will be very close, but it won’t be touching me. I forget how many hours I had to lie still for, but I was feeling pretty defeated.
I was wheeled back to the waiting room after the first round of x-rays were taken.
We remained in the hospital as I was called back every hour or so to do another round of x-rays which again were some number of hours long.
At about the 3 ½ hour mark, I started getting severe abdominal pain, it was getting harder for me to be in public with my nausea and pain growing and becoming more visible.
I went home at 1:30 p.m. when the test had finally finished meaning I had been at the hospital for 7 hours.
When I arrived home and got out of my wheelchair, my stomach was so swollen out. My rib cage was protruding outward on the left side, and I felt absolutely miserable.
Pain only increased over time and resulted in me being incapacitated in bed for 7 days due to a flare created by eating the meal for the emptying study.
The following days after the study I was in bed all day and didn’t talk. My pain levels were too high to do literally anything including speaking.
When my dad would wheel me to the bathroom, I’d be crying the whole time from the pain of my abdomen moving.
Read the next story, “New Doctors, More Tests & Still No Answers” to find the results of the GES!
Tubie Clips & Wheelchair Gear - Prepped to Face the World
As I began becoming more stable on 24-hour TPN, it allowed my body to be able to go out more often and see the world outside of my door.
On October 3rd I had planned a visit to my work to visit my boss and see what the store was up to since my body’s abrupt flare on June 24th that put me out of work. Since my dad and I were using the wheelchair so frequently, we ordered some supplies to make it easier for us to go out since my bags couldn’t fit properly on the back of the chair.
I bought on Etsy something called “Tubie Clips” which are handmade clips that clip to your clothing and have buttons to help keep your medical tubing coiled up, so it doesn’t get caught on things and accidentally get ripped out. There are so many fun patterns, and you can even match them with clothing.
On Amazon we got a wheelchair backpack that attaches to the handles of the wheelchair and has numerous compartments to store all of my medications and supplies.
Anytime my dad and I needed to leave the house, whether it was for an appointment or just to go to the park- we had to pack as if we were going to live in the desert for a week. All of these medications had to come, blood pressure and heart monitors, glucose monitors, etc. This was all because flares or spikes in symptoms could happen anywhere at any time, and we needed to have the equipment to be able to determine what was wrong to see if we could handle it there or if we needed to go back home. I had even made a laminated tag that remained on the backpack that told my dad what he needed to pack every time we went out. It was very helpful for going out and this way he didn’t forget anything.
My TPN bag was this large rectangular bag that didn’t fit on the back of my wheelchair, so it had to sit beside me in the seat. Getting into Lyfts to go to certain destinations had made my dad and I realize we needed to be better about getting in and out of cars. We would watch videos at home for how to get on/off curbs and how to load the wheelchair into the car. We’d practice in my room with me removing the legs of the chair while he would load my other bags into the “car”. This practice made perfect, and we soon became experts at the load-in and out process.
My arm’s skin began getting more irritated by the PICC dressing over time even when changing to more sensitive dressing types and trying to minimally move the dressing each week to give certain areas of skin a break. I started getting a lot of redness and blisters. My skin was always itchy, and every day became a strugglesome game of not touching my arm to scratch it. A lot of times I’d even get woken up from sleep because of the itching.
On October 5th I saw a pediatric GI specialist at another hospital to try and get more eyes on the case. They were kind and had some tests they wanted to do to look into some specific conditions that they believed might’ve been causing some of the issues. Mainly, they were concerned it was Mast Cell Activation Syndrome (MCAS). This had been the third time this condition had been brought up to me over the course of the summer-fall and I had been tested a few times with all results coming back negative. The struggle with this test is that the blood tests would only be positive if I was having a MCAS reaction at the time that the blood was being taken. We tried to measure it by when I had my hives however, they never occurred at the doctor’s office, so we were never able to “catch” it and see if they were truly stress hives or not. My labs for MCAS came back clear for the third time.
They were interested in the potential of a systemic disorder (like MCAS) or a metabolic disorder and low on their differential list was testing for IBD (Irritable Bowel Disease) since I had not had an IBD workup. They also wanted to do testing for Mitochondrial disease. Also due to my rapid weight loss they were concerned I could have developed Superior Mesenteric Artery Syndrome (SMAS) which could’ve compressed arteries in my abdomen causing severe nausea. Since my main care was at another hospital, so they gave us some more tests that we could potentially try in the future. They suggested getting an MR Spectroscopy to check biochemical changes in the brain since no one had done imaging of my brain yet either.
They were highly concerned with me being on TPN due to the extremely large risks of parenteral feeding alongside how long it had been already. They highly recommended me to trial enteral feeding and said I was likely to have secondary gastroparesis as a result of being on TPN and having minimal intake by mouth (PO).
I lent the GI team at that hospital my medical binder for 3 days where they extensively studied all of its contents to get a full picture of what was going on. This is how they came up with the plan I mentioned above.
I was sent home from my appointment feeling pretty happy with how it went and had another stool sample kit to do at home.
The next day I got a phone call that my iron infusion was scheduled for the end of January (oh myyyyyy). Throughout the months my dad and I would continuously argue for this to be moved up (which all resulted in nothing happening).
Since I had been constipated for a while since starting on TPN, I decided to take a pill called Senna to get things sped up a bit. Well, I did get my stool sample however, that pill WRECKED me. I was basically in the bathroom all day for 5 days persistently. I knew to never take that pill again. My test results came back from the stool test showing some irritation which I was like- “from that pill, no kidding!”
The day before the Gastric Emptying Study, I was constantly coming in and out of the bathroom (from the senna) and among hives, flares, nausea, and a tremor attack, I made an arm rest organizer that I sewed and attached to my wheelchair to have a place to keep my phone in. I got a pencil case and sewed some Velcro to it and attached it to my seat. It worked super well!
Read the next story to see how the longggg awaited Gastric Emptying Study went in, “G.E.S. You Are My Nemesis!”
Additional Site Information:
These posts are only reflecting my experience and therefore not the overall experiences of others who have had certain medical procedures, conditions, and/or medical devices.
• Content Warning: Blog posts cover weight, eating habits, and medical experiences which may be triggering for some readers.
• Accessible captions are available on blog post images by clicking on the white dot (for mobile devices) or clicking on the image and scrolling the mouse over the image (on laptops and computers).
• Site content is available in Spanish for readers who do not speak English or would prefer to read it in Spanish however, some jokes may not read correctly due to them being American cultural references. /El contenido del sitio está disponible en español para los lectores que no hablan inglés o que prefieren leerlo en español; sin embargo, es posible que algunos chistes no se lean correctamente debido a que son referencias culturales estadounidenses.
*All medical teams and hospital names have been excluded from all stories for privacy reasons. *