Blog Posts:
**The posts are in chronological order so the beginning is at the very bottom and the most recent is at the very top. You can navigate the posts by using the arrow at the bottom to see older posts.**
Click here to be brought to the beginning story.
Content Warning: Blog posts cover weight, eating habits, and medical experiences which may be triggering for some readers.
*All medical teams and hospital names have been excluded from all stories for privacy reasons. *
~ Scroll to the bottom to see the ‘Older Posts’ arrow to navigate past postings. ~
A Restful Winter Break
Towards the end of the semester my cough from COVID had finally left and I was able to get maintenance in to clean the carpet.
As I had approached my last week, I also had virtual rehearsals for the show I was working on.
I had been finalizing all of my medical documents that I would remain in my backpack at all times. It’s a packet for nurses, doctors, and EMTs to use that has all of the pertinent information they might need in one place.
December 17th was my first day of winter break and I spent the whole weekend in bed.
It was definitely needed, and it was nice to have a pause after such a busy fall semester.
I kept getting those ocular migraines over break but at least they weren’t occurring daily.
December 19th, I had finally gotten my genetics appointment scheduled for February (I had been struggling for a few weeks to get ahold of them).
I had also been having some CVC (central venous catheter) site pain, but I figured my lumens were probably just tugging me in some sort of way.
The following day my nurse came by to change my dressing and they found that I developed a sore next to my CVC site. The sore was caused by the stitches of my CVC rubbing against the skin.
I had begun eating again the week of finals and continued it into break however, I wasn’t able to eat very much.
I had spoken to my nurse about whether or not I should ask my dietician to up the calories in my TPN formula for January since I was going to have rehearsal every day plus school and work, and we know that I would be spending a lot of energy. They recommended I do request upped calories, so I left voicemails for my dietician.
On December 22nd I had decided to go to the hospital to visit and catch up with the physical therapists during lunch. It was such a lovely visit, and I was so glad to be able to catch up with everyone again!
December 23rd, I had tried to eat a few Smarties from a package but ended up getting sick very quickly (which is usually abnormal and a sign to stop right away). A couple hours after eating, my stomach was grumbling again, and I kept forgetting that my stomach grumbling no longer means what it used to for my body. Since I didn’t pay attention, I ate a few more Smarties.
The following day I had triggered a flare and was in bed all Christmas Eve unable to stand up fully or move about.
I had decided that I needed to be off food for a bit because I caught myself into a predicament. Since I hadn’t eaten consistently in a while (due to flares), I was flaring when I began eating again (this makes sense). So, I need to eat again to regain a tolerance *hopefully*. The issue here is the assumption I will regain a tolerance. My eating is like a downwards slope; it doesn’t improve over time it just continues to plateau and drop. Since I need time to build up a tolerance, I need time to be able to flare (weeks). Well, since I haven’t rested since my one week off in the summer, I wasn’t feeling up to letting my winter break get taken to go into a flare (since this requires a lot of energy).
And so, this is why I decided I’m going to be off food for a while because I need to spend my break resting so my body is ready to work all January, February and March (I have another show I’m working February-March).
Christmas was enjoyable and I spent it on Zoom with my family. They had mailed their gifts to me, and I had mailed mine to them.
On the 27th of December I watched the Boston Ballet’s Nutcracker with some friends which was really enjoyable, and my family and I had been playing a detective board game every night virtually together.
December 30th, I had gone to the dentist and had a great appointment! My teeth are still doing good even with not eating anything! (-I’ll take a win where I can get it!)
Once January hit, I began spending my days working on emails for my school job and prepping for my rehearsals that week. My winter break would end two weeks early in order to begin in-person rehearsals.
And of course, amongst the break time, I spent time at my desk writing seven blog posts to bring the website up to speed with where I am in my life currently.
Do I wish my break was a bit longer? Sure, but I know I’ll need to jump into everything at some point so I’m as ready as I’ll ever be ;-)
Next story coming soon!! ;-)
Entering the Holidays With A Splash!
During the early hours of the morning after my brother left (around 3-4 a.m.), my pump alarm kept going off. It went off about 3-5 times whenever I was laying on my right side (probably a line occlusion). By the time I actually woke up at 9 a.m. I had seen that my griplock had fallen off (A Velcro piece that goes on top of my dressing so I can coil my tubing around it).
My pump has never gone off in the night before.
I should’ve taken that as a sign as to the craziness that was about to ensue…
I had spent the whole morning of November 26th cleaning the house, doing laundry and showering.
I had the soccer match on and had heard a dripping sound that was louder in the living room than it was in my bedroom. I had remembered I heard this odd sound earlier in the day before I went to shower but couldn’t find where the sound was coming from.
Since I knew something had to be leaking somewhere I began standing on things and putting my ears up to the wall to figure out where it was coming from.
Aha! It was coming from the A/C unit. I opened the panel and noticed a small puddle forming on the hard floor. The drip sound would echo since the unit had some hollowness inside which was making it hard to determine where the sound was coming from.
It was a weekend, so I had called maintenance but wasn’t sure they’d be able to come by.
Luckily, they arrived at around 4 p.m. that day. They had opened up the panel, taken a look up (since that’s where the water was coming from) and sprinted out the door saying they needed to go upstairs to stop the leak.
I didn’t see maintenance again until the following day.
In that interim time, the small dripping sound went into a flowing stream sound where water was pouring out of the vents in my living room and bedroom.
It wasn’t until I saw water pooling by my bedroom door that I noticed my bedroom was flooding as well.
I sprang off the couch and started pulling out everything from under my bed into my closet. I pulled the bed away from the wall since water was getting on the bed (because the vent is above my bed). The water line kept growing so I took early precautions to take everything off the floor in case it reached the back wall by the end of the night. Some of the water had even begun spreading into my closet so I had begun moving things into my bathroom. I had tried to get ahold of maintenance and anyone else but since it was weekend and they had only sent out one person, no one was available.
I had figured the maintenance worker likely had to keep going up floors to fix the problem. Well- I was exactly right. At about 11 p.m. I heard a very loud gushing sound coming from outside my window and saw that the maintenance worker had redirected the leaking water to outside.
However, my apartment had been flooding for seven hours, the damage had already been done.
I decided to spend the night on my couch since my room was all wet and I didn’t want to walk through it.
The following morning, I woke up to see that the water seeped onto my hard floors and my carpet was warped. Maintenance came by and informed me that the leak started 3 floors above me, and I was the only apartment it flooded (it stopped on my floor).
-Wow, I love that luck.
Anyhow, they set me up with a fan that needed to run all day for the next 3 days to dry out the carpet and told me it would take a couple weeks to fix. They mentioned they’d come back to shampoo the carpets but that the hard wood would be damaged, and I needed to contact the leasing office if I wanted it fixed.
On November 28th, I woke up and felt pretty sick (but hey, that’s every day) so I didn’t think much of it. I attended my first class and ran some errands. I then went to the leasing office to have them not charge me in my electric bill for the fan running. I also requested a mold test to be done (since my A/C had the heating unit in a moist environment).
By the time I got home I was feeling very nauseous, and my medications weren’t helping. I had decided to take my temperature and saw I had a 101-degree fever.
Huh-interesting…
I had texted my family group chat mentioning I wasn’t going to attend the other two classes I had that day.
I then found out my mom and dad had both gotten COVID. The runny nose my dad thought he had on his last day at my house during Thanksgiving break, was actually COVID. My brother, however, came out unscathed-as he usually does ;-)
I had taken a COVID test, and it came back positive. Well at least I managed to not get it until now.
I spent the remainder of the day calling, emailing, and texting everyone to redo plans I had for work in the upcoming weeks.
I was bummed I was going to miss some important events for my work but was thankful it was happening in my last two weeks before the semester ended.
I wasn’t concerned at all homework-wise because I had finished all my homework for the remainder of the semester prior to Thanksgiving break (hence why I always work ahead, for scenarios such as this).
I had all the symptoms that came with COVID: chills, fever, aches, migraines, vomiting, runny nose, cough, and loss of taste (but luckily with that symptom, it didn’t impact me much).
I had a fever for about 3 days and had contacted my doctors the minute I knew about it. The nurses would call a couple times a day to check on me and they ended up prescribing me Paxlovid to help try and keep me out of the hospital.
I was still sleeping on my couch because my bedroom was still flooded, and I found out that maintenance couldn’t come by until I was completely symptom free from COVID.
The Paxlovid pills were massive which was no help to my swallowing issues and unfortunately it was unsafe to take my muscle relaxer and my oxycodone until 8 days after my 5th and last dose of Paxlovid.
I spent most of the day on my couch “in bed” and trying to attend my classes virtually when I could.
Unfortunately, my fatigue was at an all-time high since my body was already dealing with so many chronic illnesses.
On December 3rd my floor was finally dry (not clean though), so I moved back to sleeping in my bedroom.
I was still very nauseous and full every day from all the postnasal drip going into my stomach (as we know from my cold/flu from a few weeks ago). I was typically vomiting mucus 1-2 times every day.
December 6th was the first time I left my house since November 26th, and I had 2 doctor’s appointments back-to-back.
I was getting my second HPV shot, my flu shot and seeing my new primary care doctor. I had taken multiple Tylenol’s beforehand to lessen the side effects.
I hadn’t realized I hadn’t seen my new primary doctor since July of 2021 (when I was in my massive flare resulting in TPN) so they were ecstatic to see me and “how good I looked”. I was laughing because I was trying to tell them “Normally, I look even better than this!!”- since I had come into their office feeling awful from COVID.
The remainder of my finals week I stayed home and completed my assignments virtually since even after just sitting at my desk on my computer, I’d be shaking from fatigue.
I was proud that I finished another semester and couldn’t wait to rest during winter break!
See how Emma’s rest goes in “A Restful Winter Break”.
A Very ‘Emma’ Thanksgiving
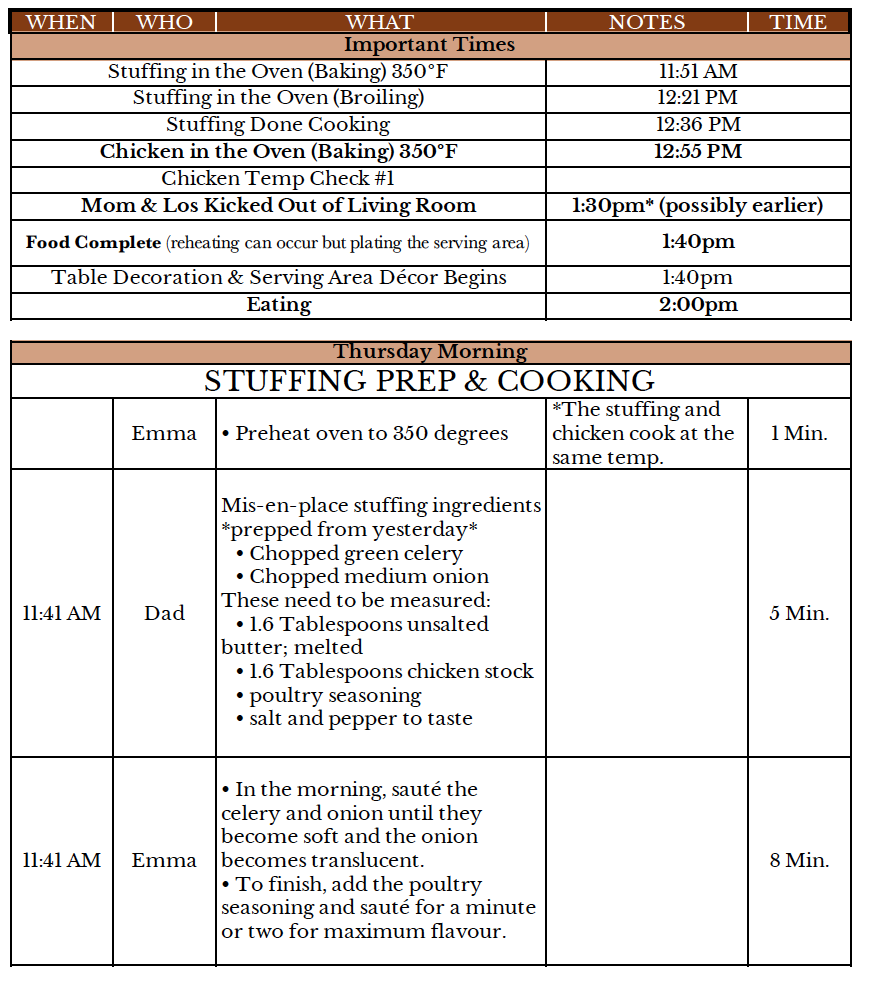
Prior to my family arriving for Thanksgiving, I had not only spent time prepping the whole house, but I had made a 20-page guidebook, multiple forms of paperwork for the actual cooking itself, pages of recommended restaurants to eat at that I knew my family would like (and that way they wouldn’t have to spend all day trying to find a place) etc.
I was so proud of my prep, and it took me a week to complete everything. I will include some of the paperwork I made below. Of course, as with any event, some hiccups came up, but I was able to get around them in the moment and the whole week went beautifully.
November 19th my brother had arrived in the evening, and I was so excited to see him. It was his first time being in Boston proper, and he had never seen my apartment before. Plus, the last time I saw him was a year ago.
The following day I had taken my brother to the grocery store, and he had mentioned he had no idea so much walking was involved in the city!! I told him that whatever we buy, we have to carry back home, and he had gotten tired by the time we made it back. I felt proud to have him see what a day in the life looked like (minus going to the grocery store) and how much was involved in it.
Later in the day I took him on another walk, and we looked inside a couple shops to take a break from how cold and windy it was outside. During our outing my brother lent me his arm on our way back home since I was having a vertigo attack and unable to keep upright. It was such a nice moment and example of how our family life has changed amongst my symptoms coming up; we adjust smoothly instead of making it a big deal.
That evening I had also made the decision to stop eating for the week since I had been having so much trouble with the cream of rice making me sick lately (as of the past month) and I was then starting to react to the Smarties as well.
The new TPN formula was working better though, because even after a full day of walking, I didn’t have any stomach grumbling!
On November 21st, I had 3 classes that day, so I wasn’t able to be home when my parents arrived at my apartment.
I couldn’t wait for my classes to be over so I could go home and see them all there. I hadn’t seen my mom since last March, and my dad since May. This was the first time our family had been all together again since last year’s Thanksgiving!
It was great catching up in the evening and watching “Dancing with the Stars” on TV together. We had so many laughs into the evening, and everyone was looking forward to the rest of the trip.
On November 22nd I went with my dad to the hospital for my second iron infusion (since I was told before I left my previous iron infusion, that I needed to schedule a second one at the front desk). When we went to the hospital, we had waited for 30 minutes to then be told I didn’t need a second iron infusion. My dad and I didn’t mind though because we had spent the 30 minutes talking about fashion.
That evening I had scheduled for the family to go to the Seaport Snowport Market which I had a feeling they’d love the winter ambience and food trucks with tons of snacks from crepes to hot chocolate. There were so many unique shops to look at and I was excited to have them see it for the first time. They absolutely loved it and loved the food which just made my heart so full.
Everyone was saying they were loving the trip and the events I had planned which made all the pre-planning time I spent worth it!
We then made it tradition that every evening, everyone would move their inflatable beds to be able to see the TV in the living room, and we’d watch “The Great British Baking Show” all together.
On November 23rd I had an appointment at 8 a.m. with my autonomic neurologist and was generally feeling very sick that day.
In the appointment we rediscussed what we had at the other appointment previously, which was to continue proceeding with trying to get IVIg approved. I was also given a paper referral for my geneticist since the doctor said they were unable to get ahold of them. I had also been given a referral to cardiology for my inflammation and chest pain to make sure it’s breathing related and not heart related.
Later that day I took my family on a walk around Beacon Hill to see all the lit-up shop windows for the holidays.
Thanksgiving morning, we were up early to watch the Macy’s Thanksgiving Day parade on TV. Afterwards we put on the world cup and had a lot of laughs as everyone was yelling at the referee on the TV.
My dad was my sous chef (to make sure I wasn’t overdoing it) and we began cooking at around 11:30 a.m. My brother was my taste tester since my dad and I both couldn’t eat the food we were cooking.
Everything was smelling amazing in the house, and I was so proud that I was able to cook something again.
I had in the schedule that my mom and brother would have to leave the apartment close to the end of the cooking so I could set up the table and make everything look nice.
After everything was set-up, my dad and I invited everyone inside and my friend had also just arrived on time to join us on their day off from work.
My family was SHOCKED at how beautiful everything looked and they were amazed at how great the food tasted!!
- Heck, even I figured it wouldn’t be that great ;-)
Everyone kept saying they were surprised the food came out so good and the chicken (we got a chicken instead of a turkey) came out perfect.
We all enjoyed our time together at the table and had lots of laughs!
After the meal, my family did the dishes for me (YAY), and I laid on the couch since I accidentally spent too much energy cooking (eh- it was worth it). They then began setting up all my Christmas decorations in my house.
We took some photos and watched more of the baking show that evening.
The following morning, we had planned in advance to do a “mini-Christmas” and exchange a gift for each other since we knew we wouldn’t be spending Christmas together again this year.
That morning my dad had woken up with a runny nose, so out of precaution, he wore a mask in the house all day.
We unwrapped our gifts and spent the day in watching more soccer matches. That evening my parents flew back to Texas and my brother left the following morning.
Everyone said it was a Thanksgiving for the books and we’d like to make it a new yearly tradition to have me host Thanksgiving for everyone.
I was so pleased with how everything turned out and that everyone had such a wonderful time.
See how Emma’s entrance into December goes in, “Entering the Holidays with A Splash!”
Thankful For Iron
In the week following my GI appointment, I had some more inflammation issues due to the humidity being 100%. I seemed to have injured the arch of my left foot (the already injured one) because it was extremely swollen one day, and I popped a blood vessel walking to class. It resolved itself two days later.
I got my new TPN formula on the 27th of October and was excited to be fully back to all lipid bags.
I was still having some stomach grumbling issues and was often getting embarrassed at school for how loud they were in class.
On November 2nd I had a hematology appointment which I was surprised I got so soon. I was referred initially but the referral never went through, so I called, and they were able to schedule me in the following day. Perhaps they have my name flagged since they know from the past that it’s better to see me sooner rather than later ;-).
It was a great appointment to see them again because the hematology team is a goofy bunch (to me personally). They spent about 10 minutes straight telling me that they don’t think I have porphyria which took everything in my being to not laugh out loud. I thought it was so cute they felt it was something they needed to tell me about when I had been trying to convince them all last year that I didn’t have this condition.
Otherwise, I had mentioned to them that I needed to schedule another iron infusion since my other iron lab test (that I forgot the name of at the time) was low. I mentioned ferritin was fine but the other one wasn’t. They went to the computer and then read my lab test result letting me know my ferritin was fine and my other iron lab test was low. They said I should get an iron infusion. – See, they like to figure it out for themselves, and I’ll take the unmentioned credit ;-)
I had sent some portal messages to my doctors that evening, and I realized my emails use my “stage manager work language” and even my appointment from earlier with hematology had it. When I had walked into the appointment, I had asked how my doctor was doing and feeling- whoops!!
Post November 2nd, I was having a lot more difficulties with my cream of rice and eating in general. My stomach would grumble more so I would respond by eating more which just created a whole slew of issues.
I would get frustrated because the hunger wasn’t resolved by eating more and I would become very weak and shaky even though my blood sugars and everything was fine.
During this two-week period, I had also been getting vertigo attacks more frequently, lots of head pressure (which I normally had and assumed it was dysautonomia related) and began having more scintillating scotomas (a type of ocular migraine).
By November 14th, I had begun doing more physical activity in my classes which resulted in more stomach grumbling (makes sense) and more shakiness from fatigue.
On the 15th I had my iron infusion which I had hoped would help with my fatigue levels (it didn’t really since the fatigue was more nutrition related).
I had also begun taking a new blood pressure medication to raise my blood pressure which didn’t seem to be working much since my blood pressure was still low.
Since the stomach grumbling issue was getting worse, I reached out to my support groups to ask other TPN users if they had experienced anything similar.
I had a group consensus that I just wasn’t getting enough calories for the energy I was spending in a day. Normal people are able to eat a snack or a meal to compensate for that energy expenditure, but my body isn’t able to. So, if I spend all my energy at 10am, the rest of the day as I use energy to walk to class, do assignments, and internally have my body continue growing, it’s all using energy I don’t have which is what was resulting in the symptoms I was having.
I reached out to my dietician to up the number of calories in the TPN to compensate for the energy I was spending. They were able to send me a new formula with upped calories the following week.
Additionally, I had also been making my “help cards” for my peers at work to have in case I go into an emergency situation in which I can’t assist myself. I had them printed on business cards and have spare in my backpack. Over the break I was going to continue making more emergency prep paperwork to keep stored in my TPN backpack at all times.
I was looking forward to the weekend since I was entering into Thanksgiving break!!! I couldn’t wait to see my family and was thrilled to be hosting Thanksgiving this year.
Read how Emma’s holiday goes in, “A Very Emma Thanksgiving”.
Victory!! On The Same Page!
Content Warning: Mentions of death.
*Additionally, these views on certain medications are solely my own within my health context and should not be reflective of the greater whole.
October 21st, 2022, the big day.
This was the GI appointment I had been preparing for since July.
I was going to make the stance on my health clear, and advocate for myself and my life.
As mentioned by the title above, I think it’s clear that my speech (that I had been working on for weeks) was clearly understood and accepted by my medical team.
I believe the best way to describe how this went, is to use my own words-the words I used for my speech.
Without further ado, here it is:
“I know that you have things that you need to fill out on your computer and that it’s a time crunch since we only have 20 minutes for this appointment, but I have some things I prepared to say to get us on the same page. I even brought a timer with me today to make sure I keep myself under 10 minutes in order to best respect your time.
The first thing, I want to bring you up to speed on what I’ve been doing in the time I haven’t seen you. I’ve been researching TPN and even joined a support group to ask other patients about their experience on TPN to gather more information on it. I even attended two online conferences for parenteral nutrition to learn about up-and-coming research and treatments that are in the process of trials, which I think is something very important to know as we continue to look forward at life with TPN.
Another thing I found interesting when meeting many patients who use TPN, was that some haven’t had line infections and have been on TPN for over 10 years. I’ve also met plenty who have gotten line infections but only got them early on in their process on TPN. I just think this is important to note here, that line infections are not guaranteed with TPN. Of course, line infection risk raises with each year that one remains on TPN, but it’s still not something that is guaranteed (and a lot of other factors can/may play into it).
Going into concerns for my liver enzymes being so elevated while being on TPN (which has thus resolved since changing to lipid and nonlipid bags), I wanted to mention to you a clinical trial being done at [NAME BLOCKED OUT FOR PRIVACY REASONS] which they are looking into entering into phase 2 of clinical trials for a medication that is supposed to help lower liver enzymes and reduce likelihood of PNALD (parenteral nutrition associated liver disease). It’s definitely something that we should be keeping in the forefront of our minds in the next 5 years, since this is something that might become an industry standard medication for those on TPN.
Next, I’ve also been researching gastroparesis as well, since I’ve personally been thinking more and more, that this is a condition I had prior to being put on TPN. I recently got a diagnosis for dysautonomia (a condition I’ve had my whole life but only figured it out now) and my medical team is also looking into diagnosing me with a connective tissue disease and in a lot of research papers there are some links to gastroparesis secondary to conditions like POTS (a form of dysautonomia) and EDS (Ehlers Danlos syndrome; a connective tissue disease).
I wanted to address the extremeness of eating small amounts of food and being sick for weeks at a time- I agree that I haven’t heard of anyone having anything like this before, however, I know one thing to be true, my body is very abnormal and only reacts with extremes to almost everything (you and I both have lots of evidence to support this). I have countless examples through years of evidence proving this statement to be true. So, if we take this information into consideration and compare my body to its past self (as we can see it documented in my journals), it does begin to make sense how it escalated over time (*noting here we are negating the “how”- we do not know how, we know parts of the “why”).
Next, I wanted to discuss my goals since this is something that we’ve never talked about. Next week I’m being moved to a maintenance formula on my TPN. Additionally, I wanted to bring attention to the fact that we only see each other for 20 minutes every 5-6 months, which means in our appointments we don’t have time to address the work that is being done behind the scenes to have me be where I am today. I’ve worked incredibly hard in those interim times to readapt my whole life to adjust and live with TPN, to live alone, go to college, etc. and I’m very proud of the progress and work I’ve done to make it so far. Because of the work I’ve done, I’m very happy with the quality of life I’ve been able to create for myself (body allowing).
On the topic of quality of life, I wanted to have the death conversation with you again, just clarifying that I care about the quality of my life over the duration. I want to let you know that I’m fully aware of everything going on because I’m constantly reminded of how risky the last resort position is. The rest of my medical team is informed of this decision. I’m not afraid of death, but just because I say that, doesn’t mean I’m ignorant towards my care of my central line- I’m just aware that death is a thing that happens to everyone (more so because of my health situation)-not just those on TPN.
Next, I wanted to clarify again why I am choosing to not pursue the trial of enteral nutrition. It absolutely in no way has to do with a fear of food. My first piece of evidence that enteral would fail is that I’ve tried the formula twice and it’s caused me to flare up (aka be immobilized). For conversation’s sake, let’s argue that this evidence isn’t conclusive enough. I have countless amounts of documentation over the past 2 years showing the experiment I conducted with myself of food over periods of time continuing to be unsuccessful. I have tried various consistencies of food over varying amounts over varying durations of time with all experiments ending with the same result- a flare. Through these experiments flares do not occur at a “set” amount of time, they just inevitably will occur over time. I’ve attempted to try and “break” the flare ending pattern and have been unsuccessful every time. Through this I’ve learned my body has developed more extreme ways to get me to stop eating (which again, I’ve tried going against which have resulted in very dangerous consequences) and I now know the flares are a warning signal to stop eating.
But let’s once again say that we’re going to ignore those two pieces of evidence for our conversation’s sake. As you mentioned to me, with your own words last appointment, the enteral feeding (again ignoring the previous facts mentioned) is literally a 50/50-coin toss on success rate. If enteral feeding is unsuccessful, I would’ve undergone surgeries and pain, periods of time of being rehospitalized and rehabilitation, taking more time off from school to then be forced to go back to TPN and the situation I’m already in. So, for me, this current position of things going well in my life and me being comfortable- why would I gamble that away? Why would I be willing to bet everything I’ve built for my life over the year on a 50/50 chance just to make my medical team more comfortable on potentially lowering one risk without knowing what others we could be causing? I want to draw our attention to the fact that I presented this scenario ignoring the evidence I supplied previously. If we take the evidence I presented into account in this scenario, the evidence all shows enteral feeding is highly likely to not work. So, for me personally, I’m not comfortable taking the 80/20 gamble (and that’s me being generous) on something that has such a low risk of being successful and impacts the whole rest of my life. However, it’s not to say I will never be up to trialing this- I am not sure where I’ll be 5 years from now, but until I personally bring it up, it will never be an option.
This is all I had to bring to the meeting, thank you for providing the space for me to bring these thoughts into the room.”
As per usual when it comes to these appointments, things still got lost in translation, but my main goal for the appointment was accomplished. I spoke my mind very clearly and got my point across.
I went home with a huge smile on my face and was eagerly waiting for the appointment notes to be published so I could review them. I always read all doctor’s appointment notes after every visit so I can see what the doctor is understanding and going away with after each appointment. Oftentimes in my case, the note will have incorrect info on it, which helps me know at the following appointment, what I need to clarify better.
My note was published later that day and attached with it was a very formal legal letter to my primary care showing that I am aware of my risks and remaining on TPN.
I was so thrilled my points came across (as reflected in their notes) and I was crying tears of joy!!
My life finally began that day.
I felt so free.
I no longer had the fear of death threats and other scenarios trying to force me into medications and trials that I wasn’t comfortable doing that would impact my whole life. I was living with a lot of “stops” because I didn’t know what was going to be chosen for me next.
I advocated for myself and was able to give myself the life I deserve!
Here’s to the start of my life!
Read how Emma’s life begins in the story, “Thankful for Iron”.
Don’t Hold Your Breath!
7:30 am on October 12th was a big day because I had a really informative virtual appointment with my autonomic neurologist about all things not GI related and what to do next.
I had brought up my breathing issues and the new development of my neck swelling which they took action to send me to other specialists to examine this further.
It already states in my diagnostic report that two doctors have a significant suspicion that I have costochondritis on top of my other issues. This was thought to be the culprit of my rib cage inflammation however, after a trial of high dose Ibuprofen leading to no change, results remain inconclusive (more on this in the story, “New Year, New Tubing”). My doctor mentioned to try pressing on my rib cage next time I had a breathing flare to see what happens.
I got a referral to pulmonology- a lung specialist to see what the breathing issues were (appointment is in February).
They also wanted to start me on a new medication since my dysautonomia issues were still disabling and medication didn’t seem to be making much of an impact. I was going to be put on a new medication called “Midodrine” which acted as a ‘full body compression sock’ to help get more blood to my brain. It had an odd dose cycle through the day since I was told to skip doses if I ever ended up laying down because it could raise my blood pressure too much.
I also got a referral to a geneticist to be tested for connective tissue disease since that is what I personally believe is causing these breathing issues (since it’s fluid inflammation in my torso making it hard and painful to breathe).
I was told we’d repeat autonomic testing the following year (since the booking is so far) to redo nerve fiber biopsies to see if my body shows a neuropathy yet.
My autonomic medical team has a strong suspicion that I am part of the small percentage of patients that my neuropathy has not spread to my peripherals yet and is still proximal. The biopsies they do are only 80% sensitive, and we have a lot of hard evidence to point to me having a small fiber neuropathy, but it just can’t be seen yet in this biopsy.
Since all of this inflammation is still so present after so many months to no avail, my doctor proposed a possible treatment I could try called IVIg. IVIg is a relatively new type of IV treatment which stands for IV immunoglobulins. It takes 80 different people’s donated immunoglobulins and has them in one bag to be injected into someone dealing with severe inflammation. Immunoglobulins get rid of inflammation and clearly my own body’s immunoglobulins aren’t doing a great job.
The IVIg, if it works, can “cure” you in the sense that it can teach your body how to make proper immunoglobulins to handle inflammation (that’s why there’s 80 different types, in the hopes that your body takes to one of them). The infusion is for 1-2 years but there is still a chance that it doesn’t work, and the body is unable to learn how to make proper immunoglobulin proteins.
The other challenge with this is that IVIg is really hard to get approved by insurance. Since I don’t have the nerve fiber biopsy to back up the reasoning for needing IVIg to my insurance, I was asked if I wanted the hospital to proceed with this treatment plan and begin building a case to my insurance.
I chose yes.
We are using other testing (inflammation blood tests, etc.) and how much my condition is disabling my life, to make a case to get this approved by my insurance.
Cross our fingers!
On October 13th, I woke up early in preparation for my virtual appointment with my new dietician. As I logged onto the portal for the visit, I received a phone call by the same person who had called me previously asking ‘who had told me that my dietician had left from my care’. I informed them that they did-they called me. They told me they messed up and that my appointment was cancelled for the day and that even though my previous dietician is no longer at the hospital, they are still on my case (since it's something with them being unable to leave my case due to the life-or-death nature of it). I was told the dietician would call the following week-great.
I had begun prepping what I wanted to talk about in my discussion with my dietician which was to ask what the “weight goal” was since I surpassed the initial weight, I was at prior to being sick. I wanted to also see if anything could be done within the TPN formula to help with these “stomach grumblings/pangs” since I had evidence to believe it was because I wasn’t getting enough calories.
My cold/flu/whatever was going on, was still happening and my abdomen was quite upset about it. Because of the large amount of mucus and postnasal drip being “digested”, my abdomen was super swollen, and it felt like a balloon that was about to pop. I constantly felt super full and I’m sure my gastroparesis was hating having so much to digest all the time. Also I had taken a COVID test on the 16th which all came back negative.
On October 18th I had a phone call with my dietician so I could address the questions I had. We decided that it was time to move me from a “weight gaining formula” to a “maintenance formula” for my TPN!! – I had no idea that we weren’t already in maintenance mode, so this felt super celebratory to me.
They also mentioned that with the maintenance formula, it’d be a reduced volume (from 2 liters to 1750mL) and we wanted to try having all lipid bags instead of the switch off since my liver enzymes are no longer looking horrendous.
That news made my week, and I was feeling much more prepared to enter into my appointment with my GI doctor with the news that we were moving to a maintenance mode.
As the big day (my GI appointment) was coming closer (*since being MOVED after I had prepped for it the month prior) I kept preparing my big speech.
I had practiced it over and over again and had even timed it! I knew that this appointment was going to be the day that I turned the tables and got to advocate for my health and my future.
Read what happens in the GI appointment in, “Victory!! On the Same Page!”
Boo! Vaccine Side Effects!
I had been looking forward to October 1st since I had reached out to one of my stage management professors about talking one-on-one on chronic illness and the industry, and they gave me a stage manager to contact who was working in the field and had a chronic illness.
I met on Zoom to speak with them and had a really fruitful and honest discussion about how their chronic conditions affected their work as a stage manager. It was helpful to get some of my questions answered and I felt better prepared moving forward as I began to work on shows again at my school.
October 2nd my inflammation issues developed a new symptom which was swelling of my neck which didn’t help with my breathing and swallowing issues. Once this started happening, I reached out to my medical team to schedule a consult to try and speed up the process of someone getting eyes on the breathing problem.
I was having a lot of issues that week with inflammation on my back and neck causing breathing difficultly which made it feel as if I was breathing through a deep fog no matter how large a breath I took.
As I began doing more in my classes, my stomach would routinely growl at a similar time every day at the end of my second class. It mostly happened on my nonlipid TPN bags, but I had made a mental note of it for myself to monitor.
On October 6th I had been invited by the physical therapy team to “have lunch” with them (I wouldn’t eat obviously, but it was a time to catch up with everyone since I had been discharged from PT in the summer). It was so awesome, and I enjoyed getting to catch up with everyone in the office. I looked forward to seeing everyone again soon!
After my lunch with the physical therapists, I went to a gynecology appointment to get someone to monitor my period irregularities. This had begun happening once I hit malnutrition, and after getting onto TPN. My body takes a long time to adjust to things plus, my TPN has affected my body in so many ways that a lot of parts of my health have been affected. Gynecology said we needed to wait until December when my body has officially had a year on this particular formula, to see if I needed to go on birth control to help with my cycles. I also got my first HPV dose done in the office since I hadn’t gotten them when I was younger.
The nurse who was giving me the shot had told me it had no side effects but that the shot itself would hurt a lot. I had mentally prepared myself for the pain and I didn’t even feel the shot when they had given it to me. The nurse was SHOCKED and had told me that I didn’t even flinch. I explained to them that I already had multiple lidocaine shots plus 2 surgeries to that arm so the pain from this vaccine was nothing in comparison.
October 7th I was up all night feeling awful and was coughing and had a stuffy nose from what seemed to be out of nowhere…
On October 8th I had felt even worse and developed a low-grade fever. I had googled and found that side effects from the HPV vaccine could give “flu-like” side effects, so I had figured that’s what had occurred.
Since I was feeling so sick, I wasn’t able to go see the ballet with a friend of mine that I had planned for the day.
The following day I continued to have a fever and on October 10th I emailed my professors that I wouldn’t be coming into class. My nurse had come to change my dressing and mentioned that the delay of the fever until the day after the shot was likely a genuine cold or flu of some sort. We figured that the HPV shot weakened my immune system enough that I was able to catch something.
Alongside having a cough, I was still having breathing pain with each inbreath and back and neck inflammation.
I attended school the next day, and continued to have a cough for the next seven weeks. You can imagine my abdomen loved that…
Read what happens next in the story, “Don’t Hold Your Breath!”
Revisiting the Foot Injury
As I was attempting to find my routine amidst classes starting, I struggled a lot with trying to get ahead.
I typically try to get at least a week ahead in homework so if I flare-up, I don’t have to stress about making up the work since it would just snowball (and there’s just too much work to make up on top of the work you have assigned currently).
My weekly calendar looks deceivingly empty with classes only on Mondays and Wednesdays leaving so many days “empty”.
I fumbled a lot with measuring my energy because after my first day of classes, I tried to do homework and ended up crashing because it was too much for my body and I should’ve used it as a rest day.
I also had an hour break in between my first and second class on Monday’s and Wednesdays and it took me a long time to accept that it had to be a rest time and not a time I worked ahead.
This semester I am taking two classes I missed when I left for medical leave in the fall of my sophomore year, along with one class I have to take now-the fall of my junior year.
Since this is rather atypical (taking them at the same time-which would only happen in a transfer student situation or a missing the semester situation), the courses are known for a heavy workload and homework load.
Through trying to navigate this all and my heavy course load, I frustratingly learned that I could only get a class ahead and not a week ahead since there was simply just too much work and not enough time.
I had many days of frustration where I’d come home and cry because I hadn’t figured out the routine yet and/or that my body wasn’t enabling me to be able to do more.
My schedule was:
Monday – Classes
Tuesday- Rest Day
Wednesday- Classes
Thursday- Rest Day
Friday- Homework
Saturday- Homework
Sunday- Homework
And that was my routine. It became frustrating also because I didn’t have any time in my schedule to do anything that “I” wanted to do.
Intermixed within all of this of course, was…. *drumroll* …. Doctor’s appointments!!!
The week of September 19th I had two doctor’s appointments on Monday and Wednesday both regarding the foot injury from two years ago.
The first appointment was on September 19th with a dermatologist to check the condition of the skin since the damage that was done with the cortisone injections back in 2020.
They were very kind and I felt so much déjà vu having to re-recite my whole medical history to a new person on the case.
It was a relatively short visit and they stated that the skin looks significantly improved since last year and that they just want to see me in three months to make sure no malignancies form under the skin.
They also recommended that I not do the tissue biopsy since they said they couldn’t see how that would benefit me in any way (within trying to find out what the injury is).
On September 21st, I had my appointment with my orthopedic surgeon-who it was so great to see after a year!
They said they were very sorry to hear about all of the GI issues, but they said the foot looked a lot better. They said they wanted me to see if it still hurts to walk without my special padding because if it still does, they wanted to consider pursuing the tissue biopsy.
They want to see me in 6 months, so the foot stuff is good to continue being on hold!!
In other news, my schedule has loosened up a little and I’ve been fitting in a couple creative activities such as drawing again (digitally and with paper), writing these blog posts, and doing a puzzle!!
My breathing has also been getting better since the humidity is dropping (since it’s getting colder outside) so I’ve been practicing walking up and down a flight of stairs for one of my classes.
I encountered a new scenario with my backpack last week that had not happened yet and I’m still working on what could’ve been a better solution to the issue.
I was on my way to class when I heard a beeping sound and eventually realized the sound was coming from me (which I was MORTIFIED).
It was my pump -of course- and I was walking really quickly in order to get to the building my class was in, to be able to shut it off. I unzipped the bag (which to reach the ‘silence’ button, I have to fully expose the whole TPN bag) and by the time I hit ‘silence’ whatever the error was, fixed itself!!- AGHHH!!!
For the rest of my two classes, I just remained in fear that it might go off again….
I figured it was likely a line occlusion or something that resolved itself when I opened the bag.
In better news, last weekend I also had callbacks for the show I’m working on in the spring which I helped run and it went great!!
It was so great to be back in a stage management position (I’m the first assistant stage manager for this show) and I got to chat a little with everyone that was called back.
And you better believe it- the following day I didn’t get out of bed until 4pm from the energy it took the previous day to do that ;-) .
So, continuing to work on getting my body used to using more energy (slowly) and also getting used to this new school routine that is starting to sink in now (plus now I have more time to do some things I want to do in the week).
See what happens next in Emma’s story, “Boo! Vaccine Side Effects!”
Summer’s Ending, Junior Year’s Beginning
The blog release went incredibly well on August 19th and was very unexpected!! A HUGE thank you to everyone who took time to visit the site!!
Unfortunately, during this time my most problematic daily symptom was my breathing issues coupled with lots of inflammation in my torso that could be seen on my back near my lungs.
I did finally receive the results to my chest x-ray which came back clear but my inflammation blood panel came back abnormal. Almost all of the results were double the maximum for inflammation.
It was finally a reason to explain what was going on!! As I continued to track when it was occurring, I knew that high humidity was the thing that would cause the inflammation to flare up.
When I had more of these breathing issues in the future, I would check with my pulse oximeter and found that sometimes my oxygenation would lower depending on how much my back was inflamed (would drop to low 90s- high 80s for about 15-20 minutes).
I had reached out to my rheumatologist to address the issue, but they said they didn’t want to handle it. I was able to schedule the soonest appointment with my autonomic neurologist (the one who ordered the blood test) and the earliest is November 23rd 2022 (so I just won’t breathe until then ;-) ).
In house news, I learned that if you rarely ever use your kitchen sink (which I don’t because I can’t cook anything to eat), then you will develop drain flies. -Lovely.
So, I spent my time getting rid of them and now I leave my drain cover on permanently in the sink.
I did restart back on cream of rice because I just needed something “heftier” than Smarties to “snack on” and luckily, I did not get vasovagal again (once again showing that my body fluctuates in making safe foods unsafe and vice versa).
By the end of August, I finally got to work as one of the stage managers for an orientation event at my school which I was so excited and nervous for-since it was the first time in over a year.
The rehearsal and performance went fantastic, and it felt so great to be back to myself again. I had brought with me a transportable stool so I could sit backstage, and it was extremely helpful.
Otherwise, my breathing issues became a daily “norm” and my abdominal issues were becoming a bit more bothersome since starting back on the rice a couple weeks prior. I was continuing to have lots of pain and bloating and began having to take nausea medication every day.
On September 2nd I had my last day at physical therapy!!! I was so excited to be discharged since I had been going for TWO YEARS!! It was such a lovely last visit, and I was really proud of the work I accomplished by the end of it all.
As the days before school starting were winding down, I was cleaning around the house and kept getting interrupted by symptoms and “doing too much” which really slowed the whole process.
One of the days I was sweeping by the kitchen and had been doing cleaning for about an hour, when I got hit with severe pain and nausea and had to lay down and not move for the rest of the day (as a result of not stopping cleaning earlier).
I had some family and friends come to visit and check in prior to school starting which was really great to catch up with everyone.
As it began continuing to rain in Boston, my inflammation was spreading to my neck which didn’t help much with the whole “breathing issue”.
My first day of school went pretty great but my body was a lot less prepared for it than I was expecting.
Since I had done summer classes, I thought my body wouldn’t have that large of a jump to make to go into 3 in-person classes on the same day (I only had class on Monday and Wednesday). After arriving home from my first class, I almost threw up from how much energy it took me to “act normal”.
I also was really not used to the weight of carrying my TPN bag with all my school supplies in it, which resulted in my backpack strap actually cutting my shoulder from the weight. (It got much better after it became the norm).
The adjustment of finding rest time and when to do work was extremely tough for me this semester but I’m glad to say, over time, it found its routine.
Read what happens next in the story, “Revisiting the Foot Injury”.
Cheers To A Year On TPN!
Wow! A whole year on parenteral nutrition!
It sounds like such a strange thing to say because I would’ve never expected something to have happened to my health that was severe enough to need this form of medical assistance.
If you are new to the blog, I encourage you to go back to the beginning of the story and find out how I got to where I am today because it can look pretty crazy initially.
As you can likely gather from my medical journey, TPN (total parenteral nutrition) was both literally and figuratively a “life-saver”.
I was first put on TPN back on August 19th, 2021 (exactly one year from today!!) because I was brought into the hospital in a state where I was very close to dying.
My primary undiagnosed medical condition had gotten so severe to where my body wasn’t tolerating any food or liquid and was doing everything it could to stop me from eating (which is known to trigger a lot of my symptoms).
My flare for that year had begun on June 24th, 2021 and lasted 7 ½ months long. It made me deteriorate quicker and more severely than previous times.
I continued to eat amongst vomiting and becoming more incapacitated to try and maintain my health as best as I could.
As weeks and months progressed, I began having daily flare attacks which included hives on my abdomen and lots of swelling, breathing difficulties from inflammation, and swallowing difficulties which resulted in me being unable to swallow my own saliva and having to spit it out into a trash can.
I had planned with my medical team to be admitted to the hospital in mid-August, but the date kept getting extended because of the surge of COVID patients entering the hospital, which made inpatient hospital beds unavailable.
I had mostly stopped eating the day before the “expected” admittance date, but the admittance got extended 3 more days which resulted in 3 more days of barely any fluids and “food” (which I was only able to lick a bit of maple syrup from a spoon to give me some energy to keep my eyes kind-of open).
Once we called 911 to take me to the hospital (since my body couldn’t wait any longer for a bed to open up), I had to wait 2 more days to start TPN (read more on this in my story “PICC Placed...?”).
My medical team saved my life and TPN gave me way more than any of us expected or anticipated.
TPN not only brought me out of my severely malnourished state, but it also helped my unknown condition in a way that none of us can still really comprehend.
TPN allowed my body to flourish and lessened my flares to a nearly non-existent amount (unless I trigger one by eating or overdoing something which causes fatigue).
I was able to return to school, travel, get a job, and have a future that I am excited for and that I feel I can still accomplish.
TPN has saved my life AND also given me back my life.
I’m very fortunate that TPN meshes really well with my body and my particular symptoms because this most definitely is not the case for everyone.
Nowadays, I’m actually having to fight for my right to have my life back and I’m having to advocate for myself against my medical team that TPN is what is right for me and my body and it’s the thing that is allowing me to flourish.
Today is in no way a day of sadness or despair, it is a day to celebrate the huge gratitude I have for my medical device and TPN for allowing me to be here today, because my journey would’ve ended a year ago without it.
Read what happens next in the story titled, “Summer’s Ending, Junior Year’s Beginning,”!
The Continuation of Inflammation
Every year, I get new symptoms that add on to my chronic illness. This is usually pretty typical of most who have a chronic illness and as time goes on, you’ll likely get new issues added into the mix.
It took me a while to realize the connections between everything, but it’ll be explained out here.
Since my previous flare, I began eating again on July 30th. I had some Smarties and had my usual issues but not to flare degrees, so I knew it was “safe” (within my definition of safe) to continue eating them.
August 1st, I spoke to my nurse about my continual breathing issues, and we discussed that it was likely they were inflammation related but we just didn’t know how or what was causing it.
August 2nd, I had taken some photos for the blog and was wearing a pair of my heels. When I had taken them off after the photo, my right foot was hurting under my sesamoids. Oh great, don’t tell me I injured the other foot too…
I thought it was odd but didn’t think about it and just tried my best to limp off both feet now because I had a more pressing pain issue elsewhere which was drawing my attention further than the foot pain.
My hands.
My left hand was as I used to say, “cramping closed” and my knuckles and thumb were extremely hard to move. I tried to just not use my hand and went about my day as best I could.
Then, my breathing pains and chest pain had crept into the party, and I was still mostly focused on my hands because they were hurting the most and it was difficult to even hold my phone to text my dad.
By the evening, my left hand was very swollen and red so I took lots of photos and sent it off to my medical team.
I got a hot pack and some Tylenol to try and help with the pain and got ready for bed.
I couldn’t even put in my retainer that night because my gums were swollen so I couldn’t fit my retainer in.
All of these things happened on the same day, but I made no connection to them until many days later.
On August 3rd I still had my foot pain, and my gums were still swollen. I didn’t have any chest pain or hand issues though.
August 4th, I had an appointment with the nurse practitioner at my primary care office who I totally freaked out with how complicated my case was.
They had also asked if anyone had responded to any of the medical messages I had sent out about my recent flares and hand issues and I had said “nope-but that’s pretty normal, I just send them out in case they want to read it,” which they were so shocked about.
It’s still true today- I never send out the messages expecting a response or help, it’s more of “I’m just letting you know this happened-do with that as you will”.
August 5th, the heatwave warning had been extended so it was really hot outside, and it was thunder storming. A perfect “storm” for rheumatological issues such as inflammation…
And wouldn’t you know, my hands, feet, abdomen, and lung area were all inflamed. I had taken photos of my back because I was having difficulty and pain breathing again for about an hour and had felt inflammation on the right side of my back close to my spinal cord that spread out across my rib cage.
My hands had some knuckle inflammation, and my feet were swollen as well.
Plus, I still couldn’t get my retainer in from the inflammation. All issues that were fine a couple weeks ago.
More signs to some sort of issue (whether I had it before or if it’s developing now) pointing to an inflammation issue.
August 7th I had decided to retry eating the cream of rice since I had taken a 2 week break from eating it and felt it was long enough to retry. I had less of the rice than usual (because it exploded in my microwave because I accidentally added too much water) so it was about an ounce of rice that I ended up eating.
I had eaten the rice at 4:30pm and at about 6:20pm that evening I began having severe pain that was enough to have me race to the bathroom. I once again had a vasovagal syncope attack (I never faint from my attacks but get the other symptoms from it).
It’s a shame- I thought the cream of rice and I were going places. :-/
August 8th, I had a virtual appointment with my autonomic neurologist, and I got the results from my autonomic testing! For my autonomic issues I have been diagnosed with dysautonomia of my parasympathetic and sympathetic nervous systems with chronic tachycardia.
This means my “fight or flight” system is dysfunctional along with my “rest and digest” system. They told me that whenever I stand up, I have a 12% drop in blood flow to my brain which is why I always feel so lightheaded all the time and usually have brain fog when standing up. My heart rate is still tachycardic so they wanted to trial me on Mestinon to see if that would help and wanted to up my dosage on the fludrocortisone since that helps with my blood pressure.
I mentioned to them the inflammation issues and they wanted me to come in the following day to get a Cytokine 13 panel done which is a blood test for inflammation markers.
August 9th was a wild day. I woke up having trouble breathing and my back inflammation was very puffy. It was super humid out and the temperature said it felt like 99 degrees and it also rained for some of the day.
I had gone to physical therapy and had the most trouble breathing than I have had in almost a year. I went home later than usual because I took so many breaks between exercises to try and breathe alongside chest pain.
I got home and told my nurse what was going on and they examined me and called my *nonexistent primary care team* and recommended for them to order a chest x-ray to make sure my Hickman didn’t accidentally puncture a lung or displace.
After my dressing change, I hopped in a car and headed to do my blood test at the hospital. They only had 1 nurse working so I spent 30 minutes in the waiting room. As I was taking the car back home, I got a phone call for an urgent appointment at my main hospital to see the on-call primary care doctor for my breathing issues.
I arrived home, changed my TPN, and headed back out the door to go to the hospital to see this doctor. It took a bit to actually get signed in since people kept sending me and another patient up and down between different floors, but I eventually got checked in.
The doctor was very pleasant and seemed extremely perplexed but fascinated with my case. They examined me and said it was a great idea to do a chest x-ray and ordered one immediately.
I was told to head over to the main hospital to get the x-ray done. I walked all the way over and the radiologist told me to go ahead and change out of my clothes and to meet them in the x-ray room.
I changed out and they said they couldn’t see the order from my doctor and that I needed to call them. -The doctor I just met minutes ago….sure, like I have their phone number…
So, I called the main primary care line, and it didn’t ring because the office was closed. I called a few more times and hit their “emergency nurse line” but every time it switched over the call disconnected.
I walked into the radiologist’s room and said, “do you have the pager number for primary care?” and they said no but that I could come back tomorrow to get the x-ray done.
Determined to get this over with I said, “No, do you really need me to go all the way back upstairs to get that order for you?” and they said they “felt bad” but I just marched off to change again.
I made it back to primary care and spoke with the receptionists to figure out the issue. The order was through, and I gave them the radiologist’s pager number to call them. They said the radiologist just didn’t look for my medical record number.
I then went all the way back to the main building and changed into the dressing gown again with the irony of me running around the hospital trying to get a chest x-ray for shortness of breath.
After the x-ray, I made it home at 9p.m. and headed off to sleep.
The following day the chest x-ray came back clear, and I was still waiting for the blood test results.
I had opened my email and been offered a stage management job to work an event at my school which I accepted!!
8/15/22 Update: The Cytokine panel came back showing almost every result abnormally elevated!! FINALLY, a test SHOWING SOMETHING!!!! Stay tuned!!
Read more about how everything goes in the article after “Cheers To A Year On TPN!”
Thoughts Filled with Cream of Rice
I had a lot of nausea whenever I’d eat the cream of rice and I often carried a trash can around with me in case I vomited but I kept eating because I enjoyed eating the rice so much.
I had trouble with figuring how much I could eat in a day so I kept eating whenever I felt like it which resulted in me feeling very sick and bloating so much that I couldn’t fit into some of my shirts.
I did have the cream of rice get stuck in my esophagus some of the time but generally if I made it with more water, it went down a bit easier.
As I continued to ignore my symptoms and keep eating more cream of rice, I began having more flare issues in later weeks.
I spent more of my free time continuing to work on the blog and doing more art drawings.
July 11th, I had just started another summer course and hadn’t figured out yet how to balance out my energy expenditure and ended up collapsing from fatigue. I also had some sort of autonomic/vasovagal attack while I was changing my TPN, but I caught it early enough that I just sat down, and my issues resolved (since I could tell my blood pressure was dropping).
By July 13th I had switched the way I was eating the cream of rice from cupcake liners to disposable paper dixie cups in order to have less dishes to do. It also helped me better measure how much I could eat in a day. I then found that I could eat up to 3 ounces of rice per day and not have to then be in bed from symptomology.
July 14th, I had changed out my TPN 2 minutes earlier than usual because the tubie clip company I get stuff from had a sale and things sell out quick, so I wanted to be able to just have to press start on my pump and then go to my computer at 6p.m.
Changing 2 minutes early meant I was not running any feeds for 2 additional minutes meaning instead of my usual disconnect time of 6 minutes, it was now 8.
From these 2 additional minutes, my body completely panicked and made my body start shaking from a drop in blood sugar.
I didn’t know what was making my body shake at the time, but I figured it was either a hunger craving, low blood sugar, or tremors.
I checked my sugars and they had dropped about 10-15 milligrams per deciliter which is why my body was all shaky. It’s so very sensitive to slight changes which is why I’m still on 24-hour TPN.
I took 2 glucose tablets and problem solved!
By July 20th I had just been having some odd symptoms that were stand alone each day. One of the days I bent over to pick something up and had a feeling that I had been kicked in the chest by a donkey for the remainder of the day. I had some other fatigue days, and more bloating.
On July 24th my flare began-great.
I had stomach pain that started intensifying but I was trying to ignore it and ended up having vasovagal syncope which I’m guessing was my body’s way of trying to get me to not ignore it.
I had some nausea medication and then tried eating a Smarties pack and after a couple pieces I felt much sicker than usual which was my hint that I was flaring and needed to stay off food for a bit.
The next day I woke up feeling awful and kept having diarrhea all day. It was a bit odd, and I figured it was likely the rice from the past few weeks (since I have gastroparesis it’s likely things are moving really slow).
I tried having a lollipop but that also made me really sick, so I just stuck to gum.
July 26th I was kept up all night and had breathing troubles which then led to chest pain and dry heaving. It was pretty weird, but I just tried my best to be comfortable, so I slept with my trashcan in my bed in case I vomited and had my backpack in bed with me too (to have my meds closer).
July 27th I was talking and began getting really fatigued from talking really quickly. I thought it was weird, so I just kept talking and ended up triggering vasovagal again.
I went to bed and couldn’t talk or move for the rest of the day from fatigue.
July 28th my breathing issues were still occurring, so I decided to call physical therapy and cancel my appointment for the next day since talking alone was making me almost faint.
By July 29th the flare seemed to have ended?... not sure but I’m still off of food just to give my body as much time to heal as possible.
In the past I have had breathing issues due to abdominal inflammation pressing on my diaphragm making it difficult for me to breathe. I figured that likely after 3 weeks of eating the rice, it created enough inflammation that I was now having breathing issues.
It’s a guess just based on what’s happened in the past, but I guess only time will tell!
Content Warning: Video shows a blood glucose test being done. Warning for needles and blood.
July 14th: A video of Emma checking her blood glucose levels while sitting on her couch with the TV on in the background. It is visible that her hands are shaking from low blood sugar making it difficult to do the glucose test.
Read Emma’s next story titled, “The Continuation of Inflammation”!
Faulty Grounds
June 29th, I woke up after sleeping for 12 hours straight and decided to spend the morning writing some blog posts for the website.
At 1p.m. I headed off to the hospital for my GI appointment (that had been canceled the previous week).
And ohhhh boyyy was this appointment interesting…
So, I always go into these appointments knowing that I’ll keep it together in the appointment and be as much of a rock as possible but when I get home, I’ll always end up crying.
I also go into the appointment always knowing that I’m going to be hit with new tough information that is assumed that I know and will be told some sort of rapid-fire plan that I have to get myself out of somehow.
And just as I expected, that’s exactly what happened.
I came into my appointment and my doctor first asked me how eating was going and if I was eating anything. I said yes (explained the Smarties and other trials) but that at the moment I was flaring a bit, so I was trying to take it easy on foods for the time being.
Then right afterwards they asked me, “so when do you want to do the liver biopsy? Now? Or do you want to wait?”
I was very confused and said “what? What biopsy-what are you talking about?”
They then proceeded to tell me that my one of liver enzymes was recently a little elevated, and they’ve done all the changes they can with my TPN, so they want to do a biopsy to see what’s going on.
I came up with my response quickly, but it was effective in slowing down their rapid-fire plans; I said, “has it been elevated consistently recently or just recently?” I asked this knowing that my liver labs only get tested once a month and they could be seeing that the enzyme for this month was high and doing all of these elaborate things instead of waiting to see if it goes down or remains the same, etc.
I then got the response, “we’ll wait then” which told my answer meaning it was likely just this month’s labs.
A lot of inferencing having to be done in these appointments and knowing the patterns of how doctors might respond and behave.
They then asked me, “when’s your next break? It’s probably winter break…”
I did not get a chance to respond before they told me what was going to happen with my care moving forward.
They said I was going to be an inpatient during winter break, and they were going to put an NG tube to trial enteral feeding. They said after the trial they’d do a surgery to put in a peg and that while I was an inpatient, they’d do the liver biopsy.
After they explained their whole little plan, I simply said, “No.”
I explained to the doctor and said I was not at all comfortable getting an NG tube because I had trialed the enteral feeding formula many times and it had resulted in large flares. And these flares mind you, were only from one sip- imagine having 24hr feeds?! I wouldn’t be able to get out of bed!
They explained to me the reason they want me to switch is once again the infection risk with central lines.
I was frustrated because I’ve had to repeat myself so many times to explain that I care about my quality of life over how much time I get. Personally, me being “alive” but being confined to my bed needing 24/7 constant care and being in pain is not living whereas having something that allows me to live and not be confined to my bed is what I prefer to choose.
After the response of me saying no and that the enteral feeding made me sick, they then quickly spat out the response of “maybe you have psychological and mental issues with food”.
I sighed after I heard this- it was clear that they said this because they were frustrated about not knowing what’s going on with my case.
They said it didn’t make sense that I got so sick from such a small amount of food and that my symptoms from it were so severe and nothing they’ve ever heard of before.
I said that it was fine that they had never heard of it before but it that in itself doesn’t make it then psychological.
I had to carefully explain my way out of how it was not a psychological issue or a fear of me eating food (I think that’s pretty evident in all of my articles where I eat).
In the past I had also been told by this doctor that I likely just didn’t have a high enough pain tolerance to deal with the pain and that I needed to handle the “slight discomfort” when eating.
So ya-I’d say I tend to get frustrated in these appointments when I hear things like this.
I kept expressing that I would not consent to do enteral feeding and we left the appointment both on different sides. They told me “I had time” and it was something to keep in the back of my mind-which honestly them saying that is already growth of them beginning to accept what’s going on with my health.
I got home and immediately started crying. I was crying out of fear because it’s such a scary feeling to feel as if you’re not in control of the decisions regarding your health and that everything I wanted to do could be taken away.
I called family and got back to a point where I could remind myself that I still have the control to make choices for my body and people can fight and argue with me about it but it’s ultimately my choice.
The following days after the appointment, I began my next set of summer courses and began researching and studying up on new medications that are in the works for parenteral nutrition related liver disease.
On July 3rd, my hunger cravings had once again come back with a vengeance and wanted “real” food. I was out of peanut butter because the brand I had been eating had their products recalled so I was searching for my house desperately for something to that effect.
It was once again a dangerous time because I knew if I couldn’t find anything to eat, I was going to eat the mashed potatoes (which is one of my flare trigger foods).
I was very lucky because I happened to find a box of unopened cream of rice. I hadn’t tried it yet and because of the hunger craving there was no time like the present!
I quickly heated up a serving of it and just mentally prepared myself on if my schoolwork would be able to be made up if this caused me to flare for a week. I said sure and grabbed a spoon and some salt and was ready to eat.
I put the rice in a bowl originally to make it, but I moved it into reusable cupcake liners because I know myself and if I had the whole bowl, I’d eat the whole bowl and then deal with the consequences later.
I put some into a cupcake liner and ate a bit and then waited (just to check for flare signs). The cream of rice tasted like liquid gold because again, I don’t eat much of anything with any flavor.
Continue reading how the cream of rice went in, “Thoughts Filled with Cream of Rice”.
Spending A Day Like Han Solo
June 9th my morning was spent with severe abdominal pain that caused me to have vasovagal syncope which was annoying. I never end up passing out from my vasovagal attacks, but it makes me close to.
The following few days I continued to try and rest as much as I could and worked on the mirror wall feature, I was painting.
I also began having issues with my TPN bags ending early… It seemed that some of them were being underfilled, so they were ending 20-30 minutes early from my change time which was causing a lot of problems symptom-wise (it took a lot of me calling my supply company over the course of weeks to try and fix this).
June 13th, I completed my mirror wall and spent some time coloring in some old drawings of mine.
I wanted to try and have as relaxing a day as I could since the following day, I was going to have all of my autonomic testing done. In the evening I decided to watch Star Wars because I had always said that the tilt tables look similar to the carbonite block that Han Solo gets frozen inside of (it really does! - google it!).
June 14th- Test Day!
I walked into the hospital at 6:50 a.m. and the testing lab wasn’t open yet. I met a doctor in the hallway who was off duty, and we spoke a little while we both waited to get into the lab.
When I finally got into the waiting room, I had many eyes on me since I was once again the youngest in the room by decades.
It was really kind because as I was walking with the nurse into the back for the test, the doctor who I had met earlier wished me good luck.
The nurse and I got along really well as they prepped me for the procedure.
We made so many jokes and I enjoyed listening to the science behind how all of the equipment worked.
I began doing a sweat test which had me stand on metal plates while my hands were on metal plates to measure how much sweat I was producing with electric currents.
I then was put onto the tilt table and had a breathing in test, a holding breath test, ankle and thigh biopsies and the tilt table + cranial doppler test.
The doctor had come in for the tilt table and biopsy portion and I kept forgetting to keep my head still for the cranial doppler because I had been trying to help out the nurse with my TPN bag.
The biopsy barely hurt which I was thrilled about because it meant I had to get 2 lidocaine shots and then they did a punch biopsy to test for small fiber neuropathies.
When they were setting me up for the tilt table test, they had to put on so much equipment on me. As they were putting on all of the equipment, a window washer landed on the window!!
The window had the blinds pulled up and the window washer looked SO CONCERNED- it was HILARIOUS!
The doctors and I all looked at each other and started laughing because the room didn’t even look like a doctor’s office it was a laboratory and we all said that the window washer probably thought they were doing child experiments.
After the tilt table test, I had completed the other two breathing tests and then had my biopsy sites bandaged by the nurse.
As I got ready to leave the nurse mentioned how nice it was to meet me and that it was rare to find someone so happy in such chronic pain. -It felt nice to have someone notice that and appreciate it .
I fell asleep when I got home because of how early I had been up for the exam.
The following day I changed out my Band-Aids because the one on my thigh gave me a blister from how sensitive my skin is!
June 16th, I woke up after sleeping another 13 hours straight and had lots of abdominal pain, so I tried to stay off food again for the rest of the day. I had also realized that the end of June was coming up meaning I had missed another period in a row (my guess was because of the flares?..)
I must have superpowers because the following day (after just writing the previous day that I had missed 2 periods) I had my period start.
The following 2 days I had continued upper abdominal pain and nausea which was getting pretty normal at this point, but it made me try to continue to stay off food.
June 21st, I had lots of weird deep chest pain and heart palpitations all day. I figured it was just my line poking me in the wrong place (because that happens a lot when I’m sleeping on the central line shoulder) but it was pretty uncomfortable to have it all day.
I was also getting ready that day to go to my GI appointment, but I got a call as I was getting ready that the appointment got cancelled. So, because of this, I spent the afternoon drawing my parent’s living room instead.
The next day I had gotten the picture frames for my living room posters, so I spent the day putting them up (which made me so fatigued BUT they look gorgeous).
June 24th, I had a dentist appointment, and it was also the one-year anniversary since my most recent flare. It was weird to think that a year ago today I had no idea that the flare would end up lasting as long as it did and would result in me being on TPN.
The dentist went really great, and I had been given a new hygienist who was super kind and we got along really well.
After the appointment I decided to go on a walk because I wanted to try and spend the day in opposite of how my day went a year ago.
I ended up walking TWO MILES which was insane, but I was really proud of myself for getting so far and making sure my walking pace was better.
June 26th, I slept 12 hours straight (you see how this is a pattern?) and decided to spend the day repainting my TV stand.
From working all day painting the stand I did have to take nausea medication in the evening, but I was proud of how well it turned out.
June 27th and 28th I had issues with my blood pressure being really low, so I had a lot of lightheadedness and fatigue.
My nurse went ahead and drew my iron labs to check to see if that was the cause of why my blood pressure had been low the past couple of days.
I spent the following day resting since I knew I had my GI appointment the following day and wanted to give my body as much physical and mental rest as I could.
See how Emma’s GI appointment goes in, “Faulty Grounds”.
When It Rains, It Pours
May 26th, I went to virtual class and had 1 Smarties pack afterwards. In the late afternoon I began having severe abdominal pain that was making me consider taking an oxycodone.
I had plans in the evening to go watch a theatre show that I was really looking forward to so I was trying everything I could to be able to go and watch it that evening.
I had tried having some gum to help with the hunger craving aspect of things, but I had to spit it out after 2 minutes because of how sick my stomach was feeling.
I laid on my couch all the way up until I had to leave to watch the show. I left at 6:30p.m. and got to spend the evening to watch the show with some friends. It was so nice getting to see them and the show was fantastic.
I ended up arriving home at 11p.m. and was so tired that I didn’t really notice any of my symptoms from earlier in the day.
The following day I woke up and was struggling a lot because of the heavy amount of pain I was in. I took some nausea medications and an oxycodone as I headed out for physical therapy.
I had also stopped taking my sodium retention pill that morning (fludrocortisone) since my tilt table test was coming up and I was asked by my doctors to start getting off of it for the exam.
Because I was off of the fludrocortisone, I could feel a lot of how fast my heart rate was because it had been kept much lower with the medication.
I got back home from physical therapy and felt like I needed to vomit all of my insides out.
I took a nap and woke up feeling just as bad as before. I went to sleep with my trash can in my bed in case I vomited.
May 28th, I realized I had missed my period for the month which was odd considering the only other times I had missed my period was while I was going through malnutrition (which makes sense). I wasn’t sure what was making it miss now…
I had really bad fatigue, had a lot of nausea and a vertigo attack in the afternoon. I sent along a message to my care team just letting them know what had been going on just to try and keep them informed.
May 29th, I woke up at 8:10a.m. after sleeping for 13 straight hours (I had fallen asleep at 7p.m. the previous day). I SPRANG out of bed to pee and took a shower. I had to take glucose tablets afterwards because I accidentally took too long again which resulted in my whole body shaking.
I had still been off of food since I was trying to recover from the flare but it’s always the absolute hardest part (and the first 4 days are the hardest).
I watched so many food videos on Instagram of food being prepared while I had cooking shows playing in the background on my TV. If a neighbor was cooking something I could identify what it was from down the hall. It helped stave off some of the cravings, but it continues to be the hardest challenge.
That evening my PICC scar suddenly had an itchy bump on it that lasted for about an hour and then went away which was weird.
May 30th in the evening, I tried for the first-time reintroducing food into my diet again because I couldn’t hold off any longer (psychologically speaking). I had 1 Smarties pack while watching a movie.
3 hours after eating it I had more uncomfortable abdominal pain, so I went to bed to try and sleep it off.
I was kept awake and didn’t end up getting to sleep until about 6 a.m. I woke up at 8a.m. because I had classes.
My stomach felt awful, so I did not eat anything for the day.
The pain and nausea were extremely heavy and during my class breaks I had to lay on the floor and moan out of pain.
The pain remained steadily increasing in symptomology throughout the day.
I tried to nap and ended up missing my alarm to take out my TPN to defrost so I had to connect to very cold TPN. Afterwards, I remained in bed trying to watch thriller movies to try and help distract myself from the amount of pain I was in.
June 1st was day 7 of the flare and I didn’t get to sleep until about 4 in the morning.
I went to physical therapy and studied for my virtual class’s exam the following day.
June 2nd, I had an appointment with my primary care physician which I had been looking forward to in order to hear their opinion of my letter from back in March (Moving Apartments, Turning 20, & Making Decisions).
After my virtual classes I headed to the hospital for my appointment. I went in and explained how good everything had been going on TPN. We once again had some more difficult conversations about the risks of TPN. They mentioned how it’s a challenging place to be because enteral feeding would make me very sick but parenteral feeding could kill me.
It was about midway through the appointment, and they then let me know that this would be my last appointment with them because they were leaving primary care.
It was tough for me to process it in that moment because I was still trying to focus on getting everything answered from my list of questions and to have them help me (for the last time I guess) persuade the GI team to keep me on TPN.
They also mentioned that they realized that TPN became my “treatment” so to speak which no one had expected but I hadn’t thought of it that way.
We finished the appointment, and they wished me good luck in all of my endeavors and hoped that I got to remain on TPN.
I arrived at home and just began crying. It was hard to have the last person who was on my side leave, and it was a tough realization knowing that I would be continuing on the battle to live my life with just me now.
They had also been one of 3 people on my case who actually had listened to me and believed me. Out of the 93 doctors I have seen I have only had 3 who have been on my side which makes it challenging to have to “argue” in a sense with the doctors to get them to believe you first in order to help you.
I spoke to a lot of family members afterwards to try and remind myself that I’m still in control of my body and to remind myself to still have the courage to advocate for myself.
The following day I was still flaring but no longer with abdominal pain just a lot of fatigue.
June 4th I was less fatigued and was able to shower and work on a new art project in my home. I was making a wall feature mirror out of picture frames that I wanted to paint blue. It was really relaxing and helped to cover the breaker box I had on my wall. I had used Velcro command strips in the case that I needed to get to the breaker box for some reason, I could get to it.
My flare continued through to June 8th. This flare was 14 days long.
See how Emma’s tilt table tests go in, “Spending a Day Like Han Solo”.
April Showers Brings May Flowers & Endoscopies
On May 14th I had gone out to the grocery store to pick up some food items to have in the house for when my dad arrived from the airport. It was so hot outside that when I got home, I had to stand in my freezer to cool down.
I tried having some Jello after returning from the grocery store but after a few bites my stomach began getting angry, so I decided to listen and not eat anything for the rest of the day.
My dad arrived from the airport at 1:40 p.m. that day and I had such a great time showing my dad all of the designs I had made in the new apartment.
May 15th my dad and I spent the day indoors and he helped me put up the rest of the peel and stick contact paper in the kitchen!
May 16th- Endoscopy Day had arrived! I felt really relaxed going into the procedure day because it was the third time I was getting it done. My dad and I left the apartment early since the elevators were getting fixed at the time that I needed to go to my appointment.
We sat in the cafeteria of the hospital and chatted away until I needed to go in for the endoscopy. At 1:30 p.m. I went in and headed to the procedure prep area. I happened to see my GI doctor in the hallway, and they informed me they would switch their procedures to be able to do mine (it was then that I didn’t realize the initial person who was supposed to do the exam wasn’t them).
As I was getting all prepped, the anesthesiologist came by to talk to me about complications (since my body seems to be a bit weird with anesthesia). It was so pleasant because the anesthesiologist came in and said “I remember you! How are you?”. They told me they had been the anesthesiologist when my central line was placed and that they remembered me because of my backpack and my high heartrate! They said I had the highest heartrate they had seen under anesthesia but that it was so stable. They said under anesthesia for my central line placement, my heart rate was steady at 130 the whole time!
I was so glad to have that heartrate info to use for other appointments to show that even under anesthesia it remains high!!
I went under super smoothly for the endoscopy which I was really thrilled about and woke up feeling nauseous but definitely not as bad as in the past. I didn’t have to use a wheelchair!!!
I walked home holding onto my dad for support and the nausea all came once I got into my building.
I was walking down the hallway heading to my apartment and I told my dad as I began speeding up towards the door that he needed to open it quickly because I was about to-
Ah, too late-
-throw up.
I threw up in my mask :-/ not the most pleasant thing…
I walked into my apartment, took off my mask and continued to throw up on the floor and myself as I walked towards a trashcan. There were little blood clots in the vomit from the procedure I had just came out of.
After I was done vomiting, I headed to bed and napped. I woke up at 6 p.m. from my alarm to change my TPN (one of the times I wish I didn’t have to do that every day) and my dad brought all of my supplies to my bed so I could change it bedside.
That evening I had SOOO many esophagus spasms and it was bothering me so much.
I knew the doctors had taken esophagus, duodenum, and stomach biopsies and I guess that was triggering my spasms but making it hurt a bit more because there were biopsies taken there.
In the evening I took some muscle relaxers and nausea medication to try and help with the esophagus spasms but unfortunately, I ended up vomiting 5 more times.
I chose to send an email to my summer class professor that I wouldn’t be attending the virtual class the following day.
The following day I was SUPER fatigued and breathing itself felt like I was climbing mount Everest. My esophagus spasms were still insane all day. I had some peanut butter in the evening since I was craving it so much.
On May 19th my pathology report from my endoscopy had come out and as I had expected (and told my doctor prior to them doing the endoscopy) it found nothing.
I attended class and had some peanut butter and jello later on in the evening.
May 20th my dad and I headed out to upgrade my phone since it was 5 years old and kept shutting down when I needed it during emergencies. I was reluctant because I prefer the older models, but I knew it was time.
My mom had also wanted me to help her redesign her living room and dining room, so I spent more of my free time working on design plans for that.
May 21st was the day my dad and I were both looking forward to the whole trip. My dad visiting this time around was the first “vacation” he had because the previous two times he visited me I was either injured and on crutches (Black & Blue, In Crutches Too) or ill in bed for 7 ½ months needing constant care (The Escalation- My Dad Enters Into the Flare). This was the first time he was here, and I wasn’t bedridden.
We went to the Museum of Fine Arts and spent the whole morning and afternoon in the museum. My dad had never been, so I was super excited to take him there.
I was proud of myself because I did pretty good standing but had to take quite a few sitting breaks. My backpack had also begun to bother me with the weight of it being on for that many hours.
We spent 4 hours at the museum!
May 22nd we were also looking forward to because I had planned a morning drawing picnic with my dad at the public gardens! I brought my picnic blanket and all of my sketching materials, and we met up with friends to hang out at the park while my dad and I drew in our sketchbooks.
It was so much fun, and our pieces came out super great!
May 23rd I was so fatigued I could barely move, and my nurse had pointed out to me that it was likely because I had spent the weekend doing things 2 days in a row. I tried to remember this for the future to better manage how much rest I was getting.
May 24th my abdominal pain was higher than usual, so I noticed it a lot more and had trouble doing my daily tasks. In the evening I said goodbye to my dad since he would be leaving very early in the morning the following day.
May 25th, I cleaned the house a little and tried to spent time resting on the couch. I had some more jello throughout the day which made my stomach unhappy, but I ignored it anyways.
It had been such a wonderful and pleasant time having my dad come and visit and even though he was technically here only because I’m not allowed to go home alone after having a procedure with anesthesia, the endoscopy felt like such a minor part of the trip and that’s why we had so many other things planned.
May 25th: A timelapse video of Emma picking up her dad’s sleeping arrangements and then collapsing on the floor from exhaustion.
Read how Emma’s health continues in, “When It Rains, It Pours”.
Revisiting the Hunger Cravings
On April 28th I was enjoying my full summer day.
Since the days were more free, I began having more hunger cravings since my body wanted to spend that free time eating because that’s what I used to do before I got sick.
I had eaten 3 of my Smarties packs all in the morning and since I had created my new “max limit rule” in order to not create a flare, my brain became frustrated towards the evening because it wanted more food.
At 7p.m. I couldn’t hold off any longer and ran into my kitchen digging through my cabinets to find food. -These are always the most dangerous times for me since I’d eat my chair if I didn’t end up finding anything (figuratively).
In my pantry, at the very top, I have instant mashed potatoes which are considered a dangerous food for me, but I hold on to them still just in case.
At the bottom, I have salt, my 5-pound bag of Smarties (yes, I ordered a 5-pound bag, so I didn’t have to keep ordering every couple of weeks), and that’s about it.
I was so happy and relieved to find that on the second highest shelf in the back, there happened to be a bag of lollipops. PERFECT!
I quickly dug around to find my favorite flavor- orange (because since being diagnosed with GERD, I have missed oranges and orange juice so much). It was just what I needed and helped solve the craving entirely.
April 29th, I started reading a new book called Surviving and Thriving With An Invisible Chronic Illness which was super refreshing to read but it also gave me the idea to start a blog! I was super excited about it and spent the rest of the working on figuring out how to make a website.
The next few days all of my attention went to this new blog!! I took photos for the site and began writing the first 4 articles. It was very relaxing, and I enjoyed coming up with the titles for all of the stories!
I had written all of the title names in advance, so I knew how to break up the stories and the list ended up being SO long!! I had so many stories I needed to write!!
May 4th my body started crashing fatigue-wise from writing and working so much on the website. I spent 3 days in bed to try and tried my best to rest while being frustrated that I couldn’t continue working on the blog.
On May 6th I made the switch back from 2 Smarties and a lollipop per day to 2 Smarties and peanut butter.
My body was once again craving something with more of a “denseness” to it, so I went to the peanut butter.
I had ordered some peanut butter that came in “To-go” cups which helped me be able to break up the amount I was eating per day. I normally had about 1/8 of one To-go cup per day.
Since reintroducing the peanut butter back into my routine, my body was not very happy about it, but my mind and taste buds were ;-) (that’s always the battle of it all).
May 7th my fatigue seemed to be better, so I kept working on the website and might’ve overdone it on the peanut butter… I ate ½ a to-go cup in a day and my body started sending warning pains, so I took it into “light consideration” as I continued deciding what to eat next.
I had ordered some gum that came in that I wanted to get to also help with the hunger cravings for the times when I wanted to eat something but couldn’t -due to a flare or because I had already eaten my max number for the day.
I got Starburst gum because it was flavored like fruits (again all things I couldn’t eat since having GERD) and I was super excited to try them since I couldn’t have mint gum (because of the GERD).
My favorite flavors were the orange and lemon. –(huh, I wonder why… ;-) )
That evening instead of eating more peanut butter, I tested out the gum. It went great and I was very excited about it!!
I then incorporated the gum into the daily routine as well to help me not overdo it on the peanut butter.
May 10th, my hunger cravings still hadn’t had enough.
I wanted more.
Oh, boy.
I went all the way to the store to get Jello.
I was up the previous night until 3a.m. digging through my pantry and watching videos of food to try and figure out what else I could potentially eat (unfortunately not the first time that’s happened).
I was brainstorming a lot with sweet foods since sugars seemed to be tolerated better because there was less to digest.
So, I also had to remember to take into consideration my swallowing issues and came up with Jello!
I went and got a sugar free (since I was having a lot of sugar already and knew I’d likely eat a lot of the jello) strawberry flavor (since some orange flavored items I do react to) because I wanted to play it as safe as possible.
I had a couple spoons immediately when I got home and oh my were they absolutely amazing.
I LOVED it.
I waited a while just to see if I had any flare-like reactions and things seemed pretty okay!!
I did get the jello stuck in my esophagus which was annoying, and water wasn’t helping it get down so that remained stuck for about an hour, so I just tried to remember for the next time that I needed to dissolve it and chew it well before swallowing.
That evening, (about the time I would be digesting the Jello because of gastroparesis) I had some minor dry heaving and just took some nausea medication to try and help.
In no way did this prevent me from eating more jello- not so sure how good or bad that is…
By May 11 my stool had been pretty weird since being on the jello, but I figured it had to do with the fact that it was the first “food” in quite some time.
I had an eye appointment that day which went really well, and I continued eating jello, peanut butter, Smarties, and gum throughout the day.
I think everyone can guess what happened next…
On May 12, I was woken up from sleep in the morning from pain. I had diarrhea all morning and had a lot of nausea which prompted me to take my nausea medication.
At 9a.m. I had my first virtual summer class which lasted until 12:45p.m. I felt really sick during my class and after it finished, I wrote that I was not going to eat anything else for the day – (which I ended up not following because I had more jello at around 1 p.m.).
I felt so conflicted because my stomach was grumbling so much out of hunger, and I felt hungry, but my abdomen was in a lot of pain already.
So, what did I choose to do?
I kept eating – (not recommended; please listen to your body)
I had peanut butter, then more jello, then more peanut butter over the course of 2 hours.
I then took a 2-hour nap and had a Smarties pack and gum.
At around 10:30p.m. that night all hell began breaking loose.
My abdomen felt as if I had been punched by someone repetitively and was hurting so badly.
I woke up on May 13th feeling absolutely miserable and started the day immediately taking nausea medication. I still felt like I had been punched in the abdomen.
I felt so miserable that I finally listened to my body and decided to not eat anything.
To help with the psychological effects of my hunger cravings, I just chewed more gum throughout the day. This helped.
My body was feeling more tolerable towards the evening from not eating anything in the day.
I was hoping I didn’t cause a flare because my dad was going to arrive tomorrow and would be staying with me for a bit while I had my repeat endoscopy.
Read how Emma’s endoscopy goes in the story, “April Showers Brings May Flowers & Endoscopies”.
Heading Into Summer & Flare Cycles
April 11th, I headed to an appointment to see a rheumatologist for the first time. It went really pleasantly which was nice, but it was apparent that there didn’t seem to be any rheumatological needs so I was told to come back any time if anything became of concern.
I had been able to drop down finally from 4 Smarties packs to 3 per day but it was still causing a lot of issues for me hours after eating.
Since there was this “delay” in symptoms, I had trouble with eating too much and causing problems later.
As school was getting close to wrapping up, I had done a lot of my finals work in advance in order to not feel overwhelmed or stressed towards the end of the semester. It was definitely immensely helpful.
It gave me a lot of time to continue working on the apartment little by little.
On April 13th I had received an important phone call that I had been waiting for- a response from someone on my medical team regarding the large letter I had sent on my birthday. My dietician had called me and said that they were proud of me for advocating for myself and approved of my decision to remain on TPN.
They mentioned that my blood labs had looked really amazing, and my weight was at such an excellent place. They could see that my quality of life was highly improved and TPN was helping me maintain that.
I also requested on the phone that my dietician ask my GI doctor for a pill prep form of a colonoscopy since 1) I knew I would not be able to drink a regular prep and 2) I wasn’t eating so it didn’t make much sense to do a regular prep.
I was so happy after that phone call because I had prepped a whole list of statements since I was fully expecting to have to argue for my reasons of why I should remain on TPN.
The call had gotten me so excited for the future that I decided to google something I hadn’t done before: “long term TPN patients” which actually came up with results I wasn’t expecting.
I was expecting to see a lot of “complication” articles and things about infections and death but surprisingly I found many articles about people who lived on TPN for 20, 30, even 40 years!
This is when I found the non-profit organization called the Oley Foundation. It was founded by a nurse and her patient who was on TPN for 50 years! FIFTY!!
I found so much support watching their YouTube videos and conferences and ended up finding so much information of so many patient cases who were on long term TPN specifically at home.
I saw that they had monthly support home parenteral nutrition groups, so I decided to join to find out more information on long term TPN use from the patient’s perspective.
April 14th, I went to my first Oley meeting which was really fantastic, and I ended up taking notes for things that I could do that were good tips and advice to know for my own central line care.
Among the group I was generally the youngest in age by decades, but it was helpful because most of everyone else had been on these forms of feeding for a double-digit number of years.
I also received a phone call from my GI doctor saying they canceled the colonoscopy because they wanted me to do a regular prep and since they knew I couldn’t they said it wasn’t important since and that they didn’t think my condition was related to anything there anyways.
I was okay with this decision because I didn’t want to do the prep, so I guess a win-win.
April 15th, I had a minor-ish flare…. I had been working on some assignments for classes and didn’t realize that I hadn’t peed in a while which I normally need to go more frequently since I have so many liters of fluid being consistently pumped into my bloodstream.
I had gotten up to pee after many hours had passed and after I was done, I collapsed to the floor with pain and nausea. I couldn’t stand up and I attributed it to the fact that when my bladder was full it likely kept my organs in a certain position and now that it had emptied, all the organs moved back to their original positions which is what was causing the pain.
Not sure but it ended up hurting for 2 days so I kept it as a reminder to myself to pee more frequently and since then I haven’t had any issues.
On April 16th I ate 1 Smarties pack that day towards the evening (since the stomach hurting thing from my bladder the previous day) and it didn’t seem to be sitting super well.
April 17th this pain continued, and I was feeling really sick. I ate another pack of Smarties at about midday (as you can tell I’m not great at the whole “not eating idea”) which made me muchhhhh sicker. I had to spend the day in bed and not do anything.
My abdomen began swelling out very noticeably and my left rib cage began protruding out more (some of my stomach is underneath it because of how my torso is) and I specifically noted that I needed to chill out on the Smarties because it was looking like my body was preparing to flare.
On April 18th I woke up and felt awful and had been kept awake all night from pain. I for once held up to my own deal of not eating anything that day and remained lying in bed for the day since I was too sick to get up. I was really bummed that I seemed to be flaring because I had plans to go see the Boston Marathon in person that day but wasn’t able to.
I continued not eating anything up until April 20th (so far, the flare had lasted 6 days).
April 21st my brain was craving food so badly so I couldn’t hold out any longer- I had to have a pack of Smarties. I even specifically wrote out in my notes “I’m sorry future Emma for any ramifications from this”. And well-did I hit the nail on the head with that one…
The following day at about midday I began getting severe abdominal pain and nausea. I took my nausea medication and tried to lie down. I still somehow ignored the fact that I was actively flaring and still had another Smarties pack that evening.
On April 23rd I woke up after sleeping for 10 ½ hours straight (my body did this usually a few days after missing a lot of sleep) and of course my bladder wasn’t loving me for that.
That day I was able to do some more though and went to the park to draw since I had been doing more of that in my free time.
The flare seemed to have calmed down after that day and went back to my usual pain levels.
I just continued to try and be more aware of my Smarties intake and even changed how I was eating them to try and lessen the amount of packs I was eating per day. By eating them more slowly, my brain felt more “full” and craved it less if it felt like I was eating it over a longer period of time.
April 27th, I had my last final exam for my last class!!! HOORAY!!!! I came home and cried out of joy for all that I had accomplished that semester and I was so proud of myself.
I did have summer classes that I was going to take in order to make up for the semester I had missed but I had a full week off before they began. I spent that time resting as much as I could in order to be ready for the summer courses.
Read how Emma’s week off goes in, “Revisiting the Hunger Cravings”.
Moving Apartments, Turning 20, & Making Decisions
March 25th- Moving Day!!!!
I was so excited for moving day to be finally here because I’ve always dreamed of living alone since I was a little kid. Since getting sick, I wasn’t sure if I’d be able to do it, but I really wanted to try.
Having my own space was something I really needed because among all of the chaos and unpredictability of my illness, I wanted to be able to control the space I’d be living in.
I had also spent 6 months planning the design for the space and had put a lot of thought into my goal of, “making the inside just as exciting as the outside” since I knew I wouldn’t be able to spend a lot of time outside of my apartment because of fatigue and flares.
I was so excited and ready for this new step in life to begin!!
I woke up early to pick up my keys and headed into the new place to set up the internet and sign some papers.
Later that afternoon my mom arrived, and I got to show her the new (empty) place!
It was also the first time I was seeing my mom since getting my central line put in (since I saw her last when I had my PICC line in).
We built the couch together and spent time bringing things from the other apartment into this one.
I was super lucky that my roommate’s mom was in town as well helping them move, and they kindly offered to help us out since my mom wasn’t in town for long and I couldn’t go up and down moving stuff.
The second day of move-in early in the afternoon we completed moving everything in!!-Yay!! Right on schedule!
I had ordered some peel and stick wallpaper that my mom helped me put up and it made the space look so cool!! Everything was coming out to how I designed it in my drafts!!
I spent a lot of time unpacking everything and often got really fatigued towards the evening from working on things.
My mom and I had a lot of fun putting everything together and finding more individualized pieces for the space.
On March 28th I turned 20!! I also had classes, so I went to them and then got home to continue decorating and designing!
I had made a sort of “gift-to-myself” for my birthday which was the edited letter to my care team that I had written back when I had the enteral feeding flare that I was saving to send on my birthday.
I had made a big decision as to where I wanted to move forward with my care, and it was the first time I was going to stand up for myself and my needs before my doctors. I have included the letter below with any privacy information redacted.
The following day I said goodbye to my roommate and her mom, and that evening said goodbye to my own mom since she was flying back the following day early in the morning.
I spent the first day alone in the new apartment feeling so overjoyed and finally at home.
I came back from classes so excited to go back to my own space to wind down and just be.
As new furniture continued to come in, I would bring it upstairs into my apartment (using a cart) and build it myself!
I loved the space, and it did everything I needed and more. I felt a lot of relief being able to have control over the space and to be able to spend time in different areas of the apartment and be creative.
My first decorating project was making the kitchen green!! I had gotten more peel and stick wallpaper and a countertop peel and stick to make the kitchen match with my theme. It took many weeks, but it was worth it!!
I still had my usual health issues, but it felt much easier to manage in the new place.
The apartment also happened to be a handicapped apartment, so it made it really easy in the case of an emergency, for EMTs to fit a stretcher into the house (and not hit things or have to move things).
It also made it really great for my wheelchair because when my dad was coming in May, we were planning on using it for my endoscopy.
I spent a lot more of my free time resting in different spots and doing more creative outlets like making a career vision board.
The house design did exactly what I wanted which was to inspire me to create- something I hadn’t done in a really long time. I was so glad to have different spaces to be able to do that in.
Read more about Emma’s end of semester in, “Heading Into Summer & Flare Cycles”.
Back in the Norm & Prepping to Move!
March 13th, I decided to order on Amazon a pack of Smarties since it seems like they were discontinued being sold at all the stores around me.
I got them and ended up eating 4 packs throughout the day which my stomach really hated me for later in the evening.
They tasted really good and were the candy I had been searching for months for.
Late in the evening my abdomen was really swollen and painful. I wasn’t able to sleep at all because I was kept up from the pain.
My plan moving forward with the Smarties was to try and limit the amount of I was eating per day, so I didn’t flare up.
I still had trouble limiting the amount I was eating per day, and I still had 4 Smarties packs the following 2 days along with some peanut butter which resulted in my body absolutely hating me.
On March 16th I finally decided to listen to my body since I couldn’t deal with the pain, so I only had 1 Smarties pack but because I had eaten a lot over the recent days, my body got upset immediately after eating them.
I spent a lot of my free time working more on interior design proposals and design plans for the new place! I had even made a 32 paged document with planning and charts for exactly how the move was going to happen, what items needed to go where in what room, etc.
The stage manager in me was so happy.
I also began ordering some of my furniture in advance (I had it all detailed out) so they would arrive at the time that my mom was in town to help me move.
My body was still trying to heal from me still eating things, so my days were spent half in pain and the other half okay.
I also spent my time prep packing my room and the rest of the items in the house so that way (according to my moving planning document), when my mom arrived, I could utilize her to help me move boxes rather than spend that time having her help pack the boxes.
It did take a lot of energy out of me, and I often overdid it and spent time in bed because I’d cause a migraine from doing too much.
On March 19th I continued packing and then took a shower- I didn’t think it through because I would’ve done this if I wasn’t sick.
Because I had already used my energy to pack earlier in the day, I had to get out of the shower because my tremors started from using too much energy.
The following 2 days I didn’t get much sleep so the day’s I tended to be more fatigued.
March 21st, I went out on a walk which was really nice to be able to do and it was my first walk alone in a really long time.
I had to take a couple sitting breaks though because my circulation wasn’t great.
On March 22nd I woke up feeling pretty nauseous and fatigued from the walk yesterday afternoon.
Because of this, I had a lot of brain fog which made me have trouble focusing and forget things. On my way to class, I forgot which class I was walking to.
When I had gotten home, I tried to rest more to try and fix the brain fog.
I had my nurse come change my dressing and they brought up a really great point as to what might’ve been the cause to my odd reactions to chocolate from a year ago. They said that since my reaction to chocolate was a vasovagal syncope attack, they said I might’ve had some sort of cardiological issue with it. Since chocolate is a stimulant and has caffeine, it could’ve been the reason I’ve had odd reactions.
In my classes we were beginning to do more creative projects which I really enjoyed and gave me the opportunity to draw again. I actually ended up writing down one of the instructions for one of the design projects and continued doing it at home in my free time for fun.
The following days I continued packing and preparing for my mom to arrive in town to help me move into the new apartment!
Read how the move goes in, “Moving Apartments, Turning 20, & Making Decisions”.
Additional Site Information:
These posts are only reflecting my experience and therefore not the overall experiences of others who have had certain medical procedures, conditions, and/or medical devices.
• Content Warning: Blog posts cover weight, eating habits, and medical experiences which may be triggering for some readers.
• Accessible captions are available on blog post images by clicking on the white dot (for mobile devices) or clicking on the image and scrolling the mouse over the image (on laptops and computers).
• Site content is available in Spanish for readers who do not speak English or would prefer to read it in Spanish however, some jokes may not read correctly due to them being American cultural references. /El contenido del sitio está disponible en español para los lectores que no hablan inglés o que prefieren leerlo en español; sin embargo, es posible que algunos chistes no se lean correctamente debido a que son referencias culturales estadounidenses.
*All medical teams and hospital names have been excluded from all stories for privacy reasons. *